This is an automatically translated article.
Acute pulmonary edema often has clinical manifestations such as: shortness of breath, blue skin, profuse sweating,... If not diagnosed and treated promptly, it can affect the patient's health.
1. What is acute pulmonary edema?
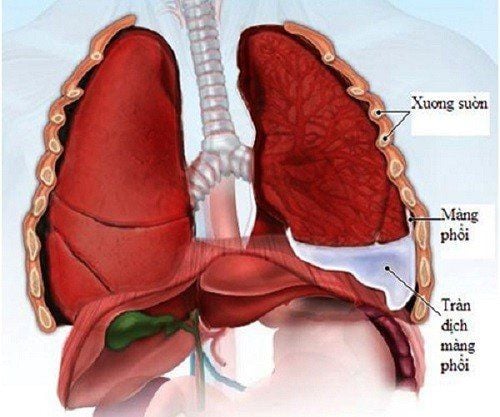
Patients with acute pulmonary edema, also known as acute asphyxia, can be caused by many different causes, causing too much water to go out of the patient's pulmonary capillaries, leading to pulmonary edema. This is an acute disease, the patient's life can only be saved if it is treated early and effectively.
Acute edema develops in 3 main stages: capillary phase, interstitial phase and alveolar phase. Based on clinical, acute pulmonary edema will correspond to the final stage of alveolar stage, with characteristic manifestations such as respiratory failure, left heart failure.

Phù phổi cấp có thể gây ra triệu chứng suy hô hấp
2. How to diagnose acute pulmonary edema?
Clinical symptoms of acute pulmonary edema include:
Shortness of breath and having to sit. Blue skin Heavy sweating Contraction of accessory respiratory muscles Cold extremities Cold extremities Feeling of suffocation The patient's cervical veins are floating in the right position. head lying position 45 degrees. In addition, patients may also experience some accompanying symptoms such as ascites, leg edema, apex of the heart may be deviated outward or below the V-shaped intercostal space in the left midclavicular line.
The majority of patients with acute pulmonary edema are caused by mitral valve disease, left ventricular failure, or some other non-cardiac condition that can also lead to acute pulmonary edema. Occurs due to imbalance in Starling's rule or functional or anatomical abnormalities of alveolar capillary membranes.
In addition, the cause of acute pulmonary edema is not only cardiac, but also can originate from intravenous anesthetic, blood infection, increased intracranial pressure, elevation, reaction due to infusion, inhalation certain toxins, shock, disseminated intravascular coagulation.
To differentiate from acute cardiogenic pulmonary edema, use the clinical setting, along with history and physical examination. In contrast to patients with acute cardiogenic pulmonary edema, the underlying cardiac disease will be detected on clinical examination or using electrocardiogram, ultrasound, or radiographs.
Diagnosis of acute pulmonary edema in patients is usually based on:
History: used to record a history of cardiovascular disease. X-ray: detect interstitial edema, alveolar edema, and most typically, diffuse butterfly-shaped edema from the navel to the periphery. Electrocardiogram: can detect signs of ischemic heart disease, patients with myocardial infarction, arrhythmia. Echocardiography: is usually required when the patient's health condition is stable, except in urgent cases where mechanical complications are diagnosed due to acute myocardial infarction such as perforation of the interventricular septum, mitral valve column, ligament rupture.
3. Treatment of acute pulmonary edema
When a patient presents with typical symptoms of acute pulmonary edema, they should be placed in a sitting position with their legs drooping, making breathing easier and contributing to a decrease in blood return. vein.
In addition, oxygen supplied to the patient should be breathed through a mask to achieve arterial PO2 above 60 mmHg. If the patient shows signs of severe depression, endotracheal intubation and ventilatory use if necessary.
The most commonly used drug today to treat acute pulmonary edema is Morfin sulfate. In the initial dose, the allowable amount of drug is 8mg given intravenously (may be through subcutaneous injection but only effective in mild cases), then can be repeated after 2-4 hours. . Morfin is a medication that increases venous capacity, reduces left atrial pressure, and can alleviate anxiety.

Phù phổi cấp cần được điều trị kịp thời để tránh những hậu quả nghiệm trọng
However, in many cases, Morfin can cause CO2 retention and reduce breathing. Therefore, Morfin is not recommended for use in patients with anesthetic-induced pulmonary edema, whose condition is usually improved by the use of an anesthetic antagonist. In addition, Morfin should not be used in patients with pulmonary edema due to neurological causes.
In addition, to treat acute pulmonary edema, the patient will be monitored based on an electrocardiogram, to ensure that the oxygen saturation through the pulse will beat continuously on the monitor.
Timely diagnosis and treatment of acute pulmonary edema is the most important factor to save the patient's life. For more information, please contact the nationwide Vinmec Health System Hotline, or register online HERE.