This is an automatically translated article.
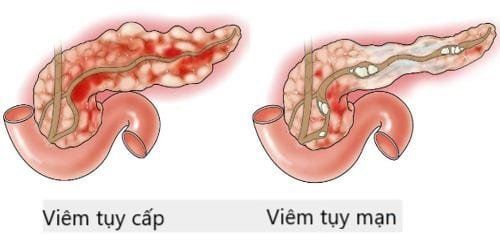
The article was consulted with Specialist Doctor I Dong Xuan Ha - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Ha Long International General Hospital.Acute pancreatitis is common in hospital emergency departments with acute abdominal pain. The disease occurs with acute inflammation of the pancreatic parenchyma, including various degrees of accompanying lesions of nearby organs and systemic complications. Acute pancreatitis can range from mild to severe and even fatal.
1. Acute pancreatitis
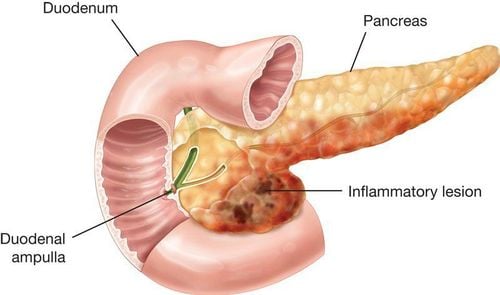
Acute pancreatitis occurs with acute inflammation of the pancreas and even adjacent tissues. The causative agent of acute pancreatitis is often caused by gallstones or prolonged alcohol consumption. The severity of acute pancreatitis can be graded on a scale from mild to severe and very severe.Gallstones cause about 40% of cases of acute pancreatitis. The main mechanism of this process is unidentified gallstones, which involve increased pressure in the pancreatic duct causing obstruction in the ampulla of vater or edema due to inflammation of the migratory stones.
High blood pressure can also lead to abnormal activation of digestive enzymes from the follicular centrosomes, thereby leading to toxic effects on the bile acids themselves on the follicular centrosomes. Acute pancreatitis due to gallstones is rare in pregnancy, and can occur in the third trimester of pregnancy.
Alcohol is also considered as one of the factors that cause acute pancreatitis. The condition occurs only after many years of alcohol use, the risk of developing pancreatitis increases with increasing levels of alcohol consumption, such as alcohol consumption 4-7 times a day for men, greater or 3 times per day for women. Furthermore, low and moderate alcohol consumption also adversely affects chronic pancreatitis. Alcohol-related acute pancreatitis can develop in a small number of alcoholics, and this factor is also thought to trigger pancreatitis.
The central cells of the pancreas, when converting alcohol into toxic substances through oxidation processes, have an effect that causes the cells to self-digest and the pancreas can become necrotic, inflamed and even cell death.
Pancreatic effects include increased levels of enzymes that destabilize lysossmal granules and zymogens, increased calcium, and activation of pancreatic astrocytes. Another cause of alcoholic pancreatitis may be an increased tendency to form protein spots in the pancreatic ducts.
In addition, there are a number of other causes of acute pancreatitis, such as:
Other obstruction: Pancreatic tumor, ampulla of Vater, worms in the bile duct, foreign body .. Due to blunt trauma to the pancreas, Peripancreatic surgery, endoscopic retrograde cholangiopancreatography.. Due to metabolic disorders, hyperlipidemia, hypercalcemia.. Due to bacterial, viral, parasitic infections.. Due to drugs, toxins.. Dominant mutations. on the autosome of the cationic trypsinogen gene. Other mutations may also be involved, but to a lesser extent and are not clinically apparent. However, the genetic condition that causes cystic fibrosis may increase the risk of recurrent acute pancreatitis as well as chronic pancreatitis. And about 10-15% of the time, no cause can be found.
2. Symptoms of acute pancreatitis
Acute pancreatitis causes persistent upper abdominal pain. The pain can radiate to the back, but it often comes on suddenly in gallstone pancreatitis or alcoholic pancreatitis. The onset of pain can last several days. While in this moment, activities such as sitting up and leaning forward can relieve pain, but coughing or vigorous movement, deep breathing will increase the pain. At the same time, common symptoms such as nausea and vomiting occurred.Patients present with severe pain along with fatigue, sweating, pulse can be up to 100 to 140 beats / min. Breathe fast and shallow. There are also some symptoms such as:
Cognitive decline, even to the point of semi-coma. Yellow sclera occurs due to obstruction of the bile duct by stones or inflammation and swelling at the head of the pancreas. Furthermore, the lungs may have limited diaphragmatic movement and potentially cause atelectasis. Patients may experience paralytic ileus and lead to decreased bowel movements and abdominal distension. Pancreatic infection or in adjacent fluid collections, fever and leukocytosis may suggest toxicity. If this condition worsens, it can lead to multi-organ failure.
3. Possible complications in case of acute pancreatitis
Acute pancreatitis can lead to different disorders at different times of illness. Acute pancreatitis is usually classified into 2 distinct stages, namely early acute pancreatitis (time to appear within a week) and late acute pancreatitis (duration of more than a week). .For the early stages are often related to the pathophysiology of inflammatory episodes. Patients with sustained systemic inflammatory response syndrome are at risk for multiple organ failure and early shock. Mortality in the early stages of acute pancreatitis as a result of multiple organ failure.
Lesser late stage of acute pancreatitis, accounting for about 20% of patients with acute pancreatitis, at this stage is characterized by a persistent systemic inflammatory response, complications may be local or more than two positions. Complications of acute pancreatitis usually include: Risk of bleeding, rupture or infection; acute fluid accumulation of necrotic tissues (acute necrosis) with the potential to cause infection; splenic vein thrombosis, pseudoaneurysmal formation, pancreatic duct obstruction leading to ascites, pleural effusion....
Accumulation of pancreatic enzyme-rich fluids that form in or around the pancreas can self-healing. But in some patients, this buildup forms pseudocysts. A pseudocyst is seen as a site of fluid accumulation usually outside the pancreas with necrotic tissue. Pseudocysts have a fibrous capsule without an epidermis, and the pseudocysts can bleed and rupture at any time.
The acute accumulation that occurs in necrotizing pancreatitis has no septum and may contain solid, liquid substances. Necrosis may include components such as pancreatic parenchyma or peripancreatic tissue. Septic necrosis may be due to necrosis that has liquefied after a period of 5 to 6 weeks. About one-third of patients with pancreatic necrosis may experience intestinal infections and have a very high incidence of this condition, even leading to death.

4. Diagnosis of acute pancreatitis
Based on clinical symptoms: Pain, vomiting, retention, distention, infection..Blood and urine tests show elevated pancreatic enzymes, signs of inflammation, infection, signs suggestive of the cause. as biliary obstruction.
Diagnostic imaging:
Pancreatic ultrasound: A simple, convenient, quick and popular method in many medical facilities, can detect pancreatitis and some causes, especially due to obstruction. However, patients with acute pancreatitis often have abdominal distention, making it difficult to perform ultrasonography, and cannot evaluate the severity of pancreatitis. Computed tomography or magnetic resonance: Computed tomography (CT) with contrast or MRI (MRI) with contrast has a higher value in the diagnosis of overcoming the weakness of ultrasound. This time allows a more detailed assessment of pancreatic lesions as well as complications of pancreatitis such as assessment of pancreatic margins, parenchymal lesions, degree of necrosis, peripancreatic fluid. Through the results of tomography, it is possible to evaluate the severity according to the Balthazar score to decide on treatment and prognosis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.