This is an automatically translated article.
The article was written by Dr. Ho Thi Anh Thu - Neonatologist, Department of Pediatrics - Neonatology - Vinmec Nha Trang International General Hospital.Acute laryngitis (VTQ) mainly occurs in children from 6 months to 3 years old, rarely in children over 6 years old. The disease usually occurs in the fall and early winter months. The disease is more common in boys than girls.
1. Causes of acute laryngitis
A common cause of laryngitis is a viral infection (parainfluenza or flu) that leads to inflammation of the larynx and trachea.
Initially, the virus enters the nose and throat and then along the upper respiratory tract to the larynx and trachea. As the disease progresses, the bottom part of the larynx and upper part of the windpipe become inflamed, narrowing the flow of air to the lungs.
The disease is caused by a virus, but there are also some cases of superinfection (co-infection with bacteria). At this time, the disease is often more severe and treatment is different from a viral infection.
2. Symptoms of laryngitis
The main symptom of laryngitis is a persistent cough and hoarseness. Laryngitis is usually mild and lasts less than a week, although some cases can be severe and life-threatening. Symptoms are often worse at night. Symptoms usually come on slowly, starting with a stuffy and runny nose. Over the next 12 to 48 hours, shortness of breath may progress and worsen. Most children have a fever, which can range from a mild 38°C to a very high 40.5°C.
Other symptoms such as rash, red eyes (conjunctivitis) and swollen glands, depending on the virus causing the disease. Dehydration can occur if a child is not drinking enough water.
As the airway narrows, stridor, noisy and rapid breathing will be heard; The child may become irritable or agitated. The more fussy the child, the narrower the airway, the more difficult it is to breathe and the more restless. When children have difficulty breathing and rapid breathing, they will be tired, exhausted and unable to breathe on their own in severe cases.
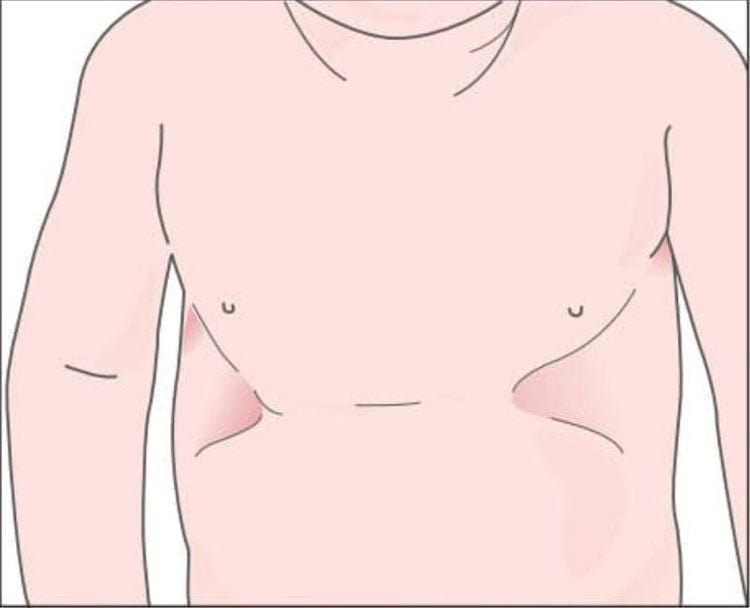
Airflow to the lungs is restricted, causing the child to become deprived of oxygen and become cyanotic. First, cyanosis may be seen on the fingertips and toenails, the rim of the ear, the tip of the nose, lips and tongue, and the lining of the cheeks.

3. Spread
Laryngitis is caused by a virus, which can be spread easily through coughing, sneezing, and respiratory secretions (mucus and droplets when coughing or sneezing). Children with laryngitis are contagious for 3 days after showing symptoms or until the fever is gone.
4. Laryngitis severity
Laryngitis can be very mild or very severe, depending on how hard the child is inhaling. The diameter of the trachea (the smaller the child, the smaller the size) and the degree of stenosis are important factors in determining the severity of the disease. It can be made worse when the baby is fussy or irritable.
4.1 Mildness Children with mild laryngitis are usually alert and have pink lips and are not breathing hard. Children can cough, the cough sounds like a barking dog. When the baby sleeps, stridor is not heard but can occur when the baby coughs or cries. Symptoms may get worse, especially at night.
4.2 Moderate Children with moderate laryngitis may have moderate stridor and labored breathing during sleep. The child may be slightly fussy, restless, irritable, and moderately short of breath.
4.3 Severity Children with severe laryngitis present with stridor and labored breathing when sitting still. Children have signs of chest indrawing and severe chest indrawing when inhaling. The child may appear restless, agitated, or tired. Cyanosis is common, initially only when the baby is moving or fussy, but gets worse to the point of appearing even when the baby is resting.
5. Diagnosis of laryngitis
Laryngitis is usually diagnosed based on the child's history and clinical symptoms, including cough, hoarseness, and stridor, which are especially common in the fall and winter. Usually no laboratory tests such as blood tests or X-rays are needed. The doctor when examining will decide the severity, and treatment depending on the level.
6. Treatment of laryngitis
Treatment of laryngitis depends on the severity and risk of progression of the disease. Children with mild symptoms and no risk factors for severe progression are usually treated at home. Meanwhile, children with moderate to severe symptoms or children at risk of severe progression should be treated in the hospital.
6.1 Mild Laryngitis Most children with mild laryngitis can be successfully treated at home. Treat your child with a warm steam bath in an enclosed room with a humidifier or in a bathroom with warm steam (which creates steam with hot water coming out of a shower).
Parents stay with the child during the sauna; A child's favorite book or lullaby can help reduce anxiety and limit crying, as this can make the condition worse.
Avoid using a humidifier with hot steam because it can cause burns. If the child's condition does not improve, parents need to take the child to the doctor.
Some supportive measures:
Put the child in a well-ventilated room by opening a window or door. Fever can be treated with acetaminophen or ibuprofen. A cough can be treated by drinking warm water to loosen mucus from the vocal cords. Warm water, apple juice, or lemon juice are safe for babies over 4 months. Smoking should be avoided in the house; Secondhand smoke can worsen a child's cough. Elevate the child's head, possibly with an extra pillow. Pillows should not be used by children under 12 months of age. Parents should sleep with children to detect symptoms of shortness of breath in time. Parents need to take their children to the doctor as soon as the symptoms get worse. Drug treatment:
Children with mild laryngitis can be treated with steam and a single dose of glucocorticoids. The most commonly used glucocorticoids are dexamethasone and prednisolone. Dexamethasone can also be given intravenously or intramuscularly when a child is vomiting a lot and is having trouble swallowing. Sometimes budesonide can be aerosolized. Glucocorticoids are effective in reducing laryngitis, usually within 6 hours after the first dose.

6.2 Moderate, severe laryngitis Moderate to severe laryngitis should be evaluated in the hospital. Severe laryngitis is a life-threatening condition and treatment should not be delayed for any reason. Treatment depends on the severity of the disease and includes:
Breathing humidified air or oxygen (if the child needs oxygen). Intravenous fluids may be needed if the child becomes dehydrated from fever or rapid breathing, both of which dehydrate the child. Monitor oxygen levels, breathing, heart rate, skin color, and alertness to assess the child's condition and response to treatment. Intubation is rarely needed in children with severe laryngitis; Less than 1% of children seen in the emergency department require intubation. Drug treatment:
Dexamethasone Dexamethasone is the drug most commonly used to treat phlebitis. It is a long-acting glucocorticoid and an effective treatment for phlebitis. It relieves laryngitis, usually within 6 hours of taking the first dose. Medications reduce the need for follow-up visits, time in the emergency room, and the dose of other drugs (eg, epinephrine).
The drug is given as an oral syrup or intramuscularly or intravenously (depending on which treatment is easiest for the child). Most only need one dose, and serious side effects are rare.
Epinephrine Epinephrine, commonly known as "adrenalin," is used by nebulizer for children with moderate to severe laryngitis. It also reduces airway inflammation and is more effective than dexamethasone. It is short-acting (two hours or less) and can be given every 15 to 20 minutes in severe cases. Inject adrenaline again after 2 hours if symptoms recur. Symptoms may recur, usually within 2 to 4 hours after treatment.
Side effects of epinephrine include tachycardia. Serious side effects are very rare. Children receiving epinephrine must be monitored 3 to 4 hours after the last dose to ensure that symptoms of airway obstruction do not recur.
Other measures:
Antibiotics, cough suppressants, decongestants and sedatives are not recommended for routine use in children with laryngitis. Antibiotics do not treat viruses, and viruses are the cause of most cases of laryngitis. Cough medicines and decongestants have not been shown to be beneficial, and sedation can mask symptoms of hypoxia and shortness of breath.
7. Measures to prevent laryngitis
Unfortunately, there is no way to prevent laryngitis. There is no vaccine to prevent most viruses that cause laryngitis. Simple hygiene measures can help prevent viral infections. These measures include:Frequent hand washing with soap and water Ideally, hands should be wet with water and plain or antibacterial soap, and rub hands together for 15 to 30 seconds. Special attention should be paid to fingernails, between fingers and wrists. Hands should be thoroughly washed and dried with a disposable towel. This is an alternative to hand sanitizer if a hand wash basin is not available. It is recommended to apply evenly to the entire hand, fingers and wrist until dry, can be used many times. When there is a sink, children should wash their hands with soap and water.

Avoid close contact with adults and children with upper respiratory tract infections This can be difficult, especially in public, but parents can try to limit face-to-face contact. Also, young children or sick children should not be sent to daycare or school as this could make others sick.
Annual influenza virus vaccine is recommended for children over 6 months of age. The flu vaccine is usually given in the fall and winter months.
8. When to see a doctor?
If at any time the child's symptoms worsen or get worse, parents should take the child to the doctor immediately :
Difficulty breathing Pale or purple skin Severe cough Drooling or difficulty swallowing Inability to speak or cry due to Difficulty breathing When breathing hear a whistling or noisy, high-pitched breathing sound when sitting or resting. Sternal depression or chest constriction Parents should take the child to the doctor when:
Fever (temperature higher than 38°C) persists. For more than 3 days Symptoms of laryngitis are mild but last for more than 7 days The Pediatrics department at Vinmec International General Hospital is the address for receiving and examining diseases that infants and young children easily Acquired: Viral fever, bacterial fever, otitis media, pneumonia in children, .... With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References article:
[1] Alberta Clinical Practice Guidelines Guideline Working Group. Guidelines to the diagnosis and management of crop. www.topalbertadoctors.org/download/252/croup_guideline.pdf (Accessed on March 20, 2013).
[2] Gates A, Gates M, Vandermeer B, et al. Glucocorticoids for crop in children. Cochrane Database Syst Rev 2018; 8:CD001955.
[3] Cherry JD. State of the evidence for standard-of-care treatments for crop: are we where we need to be? Pediatr Infect Dis J 2005; 24:S198.
[4] Vernacchio L, Mitchell AA. Oral dexamethasone for mild crop. N Engl J Med 2004; 351:2768.
[5] VSchmitt BD. Croup. In: Instructions for Pediatric Patients, 2nd ed, Saunders, Philadelphia 1999. p.70.