This is an automatically translated article.
The article is professionally consulted by Master, Doctor Le Hong Chien - Doctor of Radiology - Intervention - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International General Hospital.Percutaneous abdominal drainage is a supportive treatment procedure for acute pancreatitis, helping to effectively drain outbreaks containing inflammatory substances, cytotoxic substances, and at the same time reduce the volume of intra-abdominal fluid. Abdominal drainage reduces the number of cases of acute pancreatitis requiring surgical intervention.
1. Overview of acute pancreatitis
Acute pancreatitis is a common condition in our country. The disease can occur due to many causes such as: gallstones, roundworms; due to heavy drinking; trauma to the abdomen from the outside or from an invasive procedure; due to allergies to food, drugs, chemicals; Infection... People with acute pancreatitis often have symptoms such as:● Abdominal pain appears suddenly after a large meal, drinking a lot of alcohol. The patient has severe pain in the epigastrium, then spreading to the back or chest.
● Vomiting, nausea, pain after vomiting; Some cases have loose stools.
When examining a patient with acute pancreatitis, the abdomen is distended and the abdominal wall is stiff due to pancreatic juice causing peritonitis; edema, bleeding in the abdomen and retroperitoneum; Low back pain,... Patient has pale skin, low blood pressure, moderate or high fever, urinary, respiratory and circulatory dysfunction.
Acute pancreatitis can cause many dangerous and life-threatening complications such as:
Shock: due to hemorrhagic complications, kinin toxicity, infection
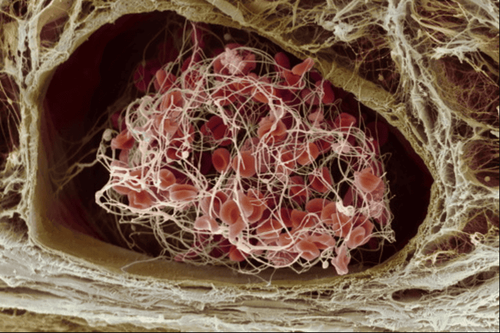
Hemorrhage in the pancreas, in the digestive tract Inflammation or distant internal organs due to pancreatic enzymes damage blood vessels
● Infection in the pancreas, the infection may be localized below the diaphragm or diffuse into generalized peritonitis.
● Acute respiratory failure
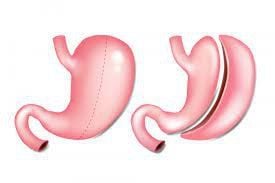
● Pancreatic pseudocyst: cysts can disappear on their own but can also persist for a long time, leading to complications of superinfection, abscesses.
Regarding treatment, the general principle in the treatment of acute pancreatitis is active medical treatment, close monitoring of the patient for indications for timely surgical intervention. Percutaneous drainage of the abdomen is an effective supportive treatment technique, helping to drain the outbreaks containing inflammatory substances, cytotoxic substances, and at the same time reducing the volume of intra-abdominal fluid. Abdominal drainage limits the spread of necrosis after surgery, limiting infection. The reduction in intra-abdominal pressure due to peritoneal drainage also improves visceral function. Percutaneous drainage of intra-abdominal fluid has reduced the number of cases of acute pancreatitis requiring surgical intervention.

Viêm tụy cấp có thể gây suy hô hấp cấp
2. Abdominal drainage technique in acute pancreatitis.
2.1. Indications for abdominal drainage in acute pancreatitis
Abdominal drainage in acute pancreatitis is performed when ultrasound or CT of the abdomen reveals free or localized fluid in a location where favorable percutaneous drainage can be performed. The outbreak is in direct contact with the abdominal wall, and the needle can be easily inserted into the outbreak.Abdominal drainage should be considered with caution in patients with uncorrected coagulopathy (platelets <50 G/l, INR >1.5).
Bệnh nhân rối loạn đông máu cần được sự chỉ định của bác sĩ khi dẫn lưu ổ bụng
2.2. Preparation for performing abdominal drainage in acute pancreatitis
● The crew performed the procedure of washing hands, wearing clothes, and wearing gloves.● The patient is instructed to lie on his back, with his head above his feet, to breathe oxygen and use sedatives to relieve pain. After that, the nurse carried out a monitor to monitor the pulse, blood pressure, SPO2 and mechanical ventilation parameters. The patient's abdomen is cleaned, disinfected with alcohol and betadine.
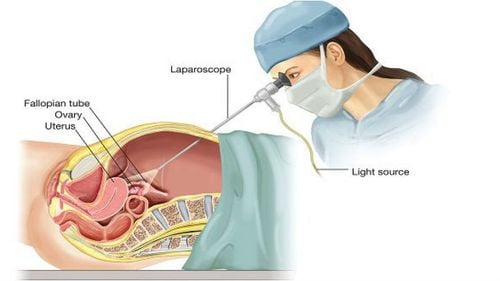
● The ultrasound machine is placed on the opposite side of the puncture site. The doctor uses ultrasound to re-determine the location to be drained. Disinfect the puncture site with 10% Betadine solution, cover with sterile sheets.
● The doctor uses a 22 or 25 guage needle, local anesthetic with 1% lidocaine. Conducting anesthesia from shallow to deep, gradually numbing layer by layer, both anesthetic and suction.
● The doctor's left hand repeats the ultrasound procedure to determine the exact position, then turns to the assistant doctor to hold the ultrasound probe in place. The surgeon's right hand holds the puncture needle under the guidance of the ultrasound probe, holding the needle perpendicular to the abdominal wall. Simultaneously insert the needle and vacuum until the tip of the needle passes through the abdominal wall, through the peritoneum, and aspirates the fluid.
● The assistant doctor keeps the ultrasound probe in place. Meanwhile, the doctor performs the procedure to transfer the needle from the right hand to the left hand. The doctor's right hand holds the guide wire of the catheter inserted into the needle. Observe the ultrasound screen, when the lead is found in the abdomen, pull out the needle and keep the lead intact.
● The doctor uses a knife to make an incision in the skin at the puncture site. Insert the abdominal wall dilator gently through the lead, withdraw the dilator and insert the catheter until fluid is seen, then withdraw the lead.
● Connect the catheter to the negative pressure drainage system, fix it, take the fluid for microbiological and biochemical tests.
3. Possible complications during abdominal drainage
Possible complications when draining the abdomen include: bleeding, intestinal puncture, drainage blockage, infection, leakage of abdominal fluid,... Depending on the accident encountered, the team will have a direction. suitable handling. Of these, bleeding is less common and may be due to the pancreatitis itself rather than from the drainage procedure. For intestinal injuries caused by a perforated catheter, the lesion usually heals on its own without intervention.The foot of the drainage tube will be changed and cleaned daily. When the amount of peritoneal fluid is less than 30ml/day, the drain is removed. In case of severe acute pancreatitis, it is necessary to measure the intra-abdominal pressure before and after catheterization.

Bệnh nhân được gây tê trước khi tiến hành dẫn lưu ổ bụng
Master. Dr. Le Hong Chien has many years of experience working in the field of diagnostic imaging and interventional radiology (endovascular intervention and extravascular intervention). Before being a Doctor of Diagnostic Imaging - Intervention at Vinmec Times City International Hospital, Dr. Chien was a Doctor at the Department of Diagnostic Imaging, Hospital 19.8 - Ministry of Public Security and Hong Ngoc General Hospital. .
If you have a need for medical examination by modern and highly effective methods at Vinmec, please register here.