This is an automatically translated article.
The article was written by Specialist Doctor I Vo Khac Khoi Nguyen - Orthopedic Trauma Doctor, Department of General Surgery - Vinmec Central Park International General Hospital.
The rates of falls and fractures in patients with type 1 and 2 diabetes are increasing. People with diabetes often have high blood pressure, joint pain, etc. The use of drugs such as insulin, antihypertensive drugs, pain relievers increases the risk of falls in diabetics. After a fall, mortality in patients with diabetes increases because of cardiovascular events and pneumonia. Therefore, the issue of preventing falls in people with diabetes is very important and should be taken care of.
1. Why is it important to prevent falls in people with diabetes?
The number of elderly people is increasing worldwide, especially in developing countries. Falls are a major problem in the elderly as they are a major cause of morbidity and mortality. Complications from falls reduce mobility, cause serious injury, and increase the cost of medical services. Diabetes is a very common disease in the elderly. The current burden of diabetes is greatest in the population over 65 years of age. This is the group that spends half of the direct medical costs for diabetes. As diabetes increasingly becomes a disease of the elderly, the associated complications must be properly intervened and taken care of. This complication includes cognitive dysfunction and physical disability, falls and fractures, as well as other geriatric syndromes in the elderly.
Diabetes is a predictor of fall risk. Several studies have recognized that older adults with diabetes have a higher risk of falls than those without diabetes. Diabetes-related complications such as peripheral neuropathy, decreased vision, diabetic foot ulcers, and impaired kidney function are potential mechanisms leading to falls. Reduced balance, muscle strength, and gait disturbance are also conditions associated with diabetes complications and risk of falls.

The consequences of falls are more severe in the elderly with diabetes. Reasons include slower wound healing, delayed recovery from falls, a higher likelihood of fractures, bone mineral depletion, and age-related loss of endurance.
Based on these reasons, the rate of falls in the elderly with diabetes will be higher than in the elderly in general. While the fall rate in the elderly community is generally around 30%, the fall rate among elderly diabetics is as high as 78% in urban areas and 43.7% among diabetic elderly living in urban areas. countryside.
2. Diet
Proper nutrition helps control blood sugar well and provides energy for the body. Balanced nutrition and energy and blood sugar control are two seemingly simple but very important aspects. Undernutrition currently accounts for 10% of people living in the general population and 65% of people with chronic diseases.
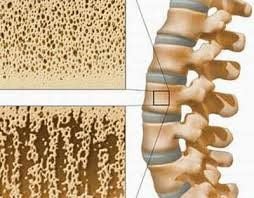
Proper nutrition helps maintain muscle mass, contributes to the prevention of osteoporosis, increases flexibility for movement organs. In the elderly, additional attention should be paid to leucine supplementation due to its anabolic effects on cell signaling and increased muscle protein synthesis.
Protein supplementation (but not other dietary interventions) especially combined with exercise markedly improves leg muscle strength reducing the risk of falls.
3. Strength training
Physical exercise helps to increase flexibility and endurance for the body, helps reduce joint pain and is one of the three pillars to help control blood sugar in the treatment of diabetes. Physical exercise should be appropriate to the age and ability of the body. Care should be taken to avoid musculoskeletal injuries. Regular daily exercise is also very important. Exercises should be consulted with a doctor to suit the individual medical condition.

4. Blood sugar control
Blood sugar control is an important key to solving the problem of falls as well as the complications of diabetes. Glycemic control needs to be on both extremes: preventing hyperglycemia beyond the therapeutic goal and preventing hypoglycaemia.
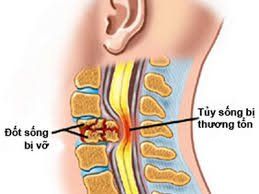
Uncontrolled hyperglycemia causes complications of diabetes such as peripheral neuropathy, vision loss, diabetic foot ulcers and impaired kidney function. These complications are potential mechanisms leading to falls.
Conversely, sudden episodes of hypoglycemia also cause falls and fractures. More dangerously, hypoglycemia can lead to coma and irreversible brain damage, causing lifelong disability.
5. Vitamin D Supplement
There is strong evidence that vitamin D supplementation is beneficial for the body. Supplementing with vitamin D not only improves muscle strength, but also reduces the frequency of falls. A daily supplement of 700–1000 IU of vitamin D reduced the risk of falls by 19% while a lower daily supplement (200–600 IU) had no effect.
High levels of vitamin D (22.5–94 nmol/l) help maintain bone mineral density. In addition to its effects on bones, vitamin D also has effects on muscles. Maintaining normal vitamin D levels improves motor function, muscle performance and strength, and reduces the risk of falls.
Therefore, people who take vitamin D supplements > 700 IU daily and have vitamin D levels > 40 ng/ml have less muscle dysfunction, less bone loss, less falls and fractures.

6. Detect and treat eye diseases
Visual impairment is an important determinant of falls in the elderly. In diabetic eye complications, retinopathy is significantly associated with falls in the elderly. Diabetic eye complications are a warning sign to screen for other vascular complications caused by diabetes.
In summary, diabetes creates an enormous medical burden. Falls in patients with diabetes are an important event with increased morbidity and mortality in the elderly. Fall prevention in people with diabetes is very important to prevent this event.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.