This is an automatically translated article.
The article was professionally consulted with Master, Doctor Le Hong Duong - Anesthesiologist - Department of General Surgery & Anesthesia - Vinmec Hai Phong International General Hospital.Endotracheal anesthesia is a technique of general anesthesia with intubation to help control breathing during surgery and resuscitation after surgery. Endotracheal anesthesia is an anesthetic method used during laparoscopic resection of bladder neck polyps.
1. Laparoscopic surgery to remove bladder neck polyps
The bladder is another name for the bladder, this is the place where urine is secreted by the kidneys and excreted through the urethra. Bladder neck polyps are formed due to an overgrowth of the urinary tract mucosal tissue at the bladder neck. People with bladder neck polyps often have symptoms such as:
Hematuria occurs suddenly, without pain, often recurs; Dysuria, dysuria, urinary frequency Pain in the pelvic region, low back pain when urinating, bladder neck polyps can be diagnosed through clinical examination combined with imaging techniques such as abdominal ultrasound, Computed tomography, endoscopy with biopsies for pathology,...
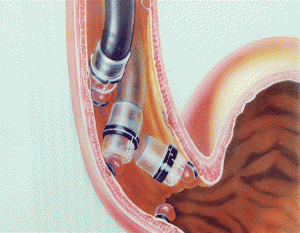
Laparoscopic bladder neck polypectomy is a commonly performed treatment method today. The bronchoscope is inserted through the mouth and urethra under the guidance of the camera into the bladder. The doctor will monitor the acquired image, use the instrument to approach the polyp location and proceed to remove it. Laparoscopic bladder neck polypectomy has many advantages such as less invasive, quick recovery time, few complications, patients recover quickly after surgery, shorten hospital stay.

Endotracheal anesthesia is one of the anesthetic methods used in bladder neck polypectomy. Endotracheal anesthesia is a technique of general anesthesia with endotracheal intubation for the purpose of respiratory control during surgery and postoperative resuscitation. This is a difficult technique, so the technique is not performed if the patient does not agree or the medical facility does not have enough anesthesia and resuscitation facilities, medical staff are not proficient in the technique.
2. Preparation for endotracheal anesthesia for laparoscopic surgery to remove bladder neck polyps
The person who performs the technique of endotracheal anesthesia for laparoscopic surgery to remove bladder neck polyps is a doctor, a nurse specializing in anesthesiology and resuscitation.
Necessary facilities to perform endotracheal anesthesia include:
Anesthesia machine system with breathing, hand squeeze oxygen source, vital function monitor (ECG indicators, arterial blood pressure, SpO2, etc.) EtCO2, breathing rate, temperature), defibrillator, suction machine,...; Laryngoscope, endotracheal tube of various sizes, suction tube, mask, squeeze balloon, oropharyngeal cannula, Magill pliers, soft mandrin; Lidocaine 10% spray, Salbutamol spray; Means to prevent difficult intubation: Cook tube, laryngeal mask, flexible bronchoscope, tracheostomy kit, mouth opener...

3. Endotracheal anesthesia procedure laparoscopic surgery to remove bladder neck polyp
3.1. Steps to conduct endotracheal anesthesia laparoscopic surgery to remove bladder neck polyps
After checking the records and examining the patient, the anesthesia team will have the patient lie on his back on the operating table, breathe 100% oxygen with a flow rate of 3-6 liters/minute at least 5 minutes before the induction of anesthesia. Install the monitor, set up the line and perform pre-anesthesia (if necessary).
Then perform induction of anesthesia with drugs:
Sleeping pills: can use anesthetic drugs such as intravenous anesthetics (propofol, etomidate, thiopental, ketamine,...), volatile anesthetics (sevoflurane, Isoflurane). ,...) Painkillers: fentanyl, sufentanil, morphine,... Muscle relaxants: rocuronium, succinylcholine, vecuronium,... are used if necessary. The condition for intubation is that the patient sleeps deeply and has enough muscle relaxation (in most cases). There are two techniques that can be used for endotracheal intubation: oral intubation and nasal intubation.
Oral intubation technique:
The doctor (or nurse specialist in anesthesiology) opens the patient's mouth, inserts the laryngoscope to the right side of the mouth, moves the tongue to the left, pushes the light deep, coordinate with the right hand to press the cricoid cartilage to find the epiglottis and glottis. Perform rapid induction of anesthesia and Sellick maneuver in case of full stomach (pressing the cricoid cartilage 20-30kg as soon as the patient loses consciousness until the intubation is complete).

Pass the endotracheal tube gently through the glottis, stopping when the balloon of the endotracheal tube passes 2-3cm through the vocal cords. Remove the laryngoscope, then inflate the endotracheal balloon. The doctor will listen to the lungs and check the EtCO2 results to see if the endotracheal tube is in the correct position. If it is in the correct position, the doctor will secure the tube with tape and place the cannula in the mouth to prevent biting the tube (if necessary). Nasal intubation technique:
The doctor chooses the side of the nose that will intubate the trachea, drop vasoconstrictor drugs such as naphazoline, xylometazoline... into the nose. Select an endotracheal tube of appropriate size, insert an endotracheal tube lubricated with lidocaine grease through the nostrils. Open the patient's mouth, insert the laryngoscope to the right of the mouth, slide the patient's tongue to the left, push the lamp deep, and coordinate with the right hand to press the cricoid cartilage to find the epiglottis and glottis. In favorable cases, proceed to gently insert the endotracheal tube through the glottis, stopping when the balloon of the endotracheal tube passes 2-3cm through the vocal cords. Using Magill pliers to guide the tip of the endotracheal tube into the correct glottis, the assistant pushes the endotracheal tube from the outside in difficult cases. Gently withdraw the laryngoscope, then inflate the endotracheal balloon. The doctor checks that the endotracheal tube is in the correct position by listening to the lungs and checking the EtCO2 results. Secure the endotracheal tube with adhesive tape. If the above two procedures are unsuccessfully performed, the team will apply the difficult endotracheal intubation procedure.
To maintain anesthesia during surgery, the patient will be given intravenous or volatile anesthetics, pain relievers and muscle relaxants (if needed). Respiration is controlled by machine or hand squeeze. The depth of anesthesia will be closely monitored based on parameters such as heart rate, blood pressure, sweating, tearing (PRST); MAC, BIS, Entropy.

3.2. Criteria for extubation
After the laparoscopic polypectomy is completed, the endotracheal tube is removed when the patient meets the following criteria:
The patient is awake, can follow orders, breathes spontaneously, and has a respiratory rate within the limits. normal term. Self-elevating head for more than 5 seconds, TOF >0.9, stable blood pressure, body temperature >35 degrees Celsius. No complications of anesthesia and surgery.
4. Possible complications during endotracheal anesthesia laparoscopic surgery to remove bladder neck polyps
4.1. Reflux of gastric juice into airway
If the patient has digestive juices in the oral cavity and airways, the anesthesia team will immediately drain the fluid, let the patient lie down with his head low and tilt his head to the side. Promptly intubate the endotracheal tube and clear the airway. Patients will be closely monitored after surgery to prevent lung infections.
3.2. Hemodynamic disorders
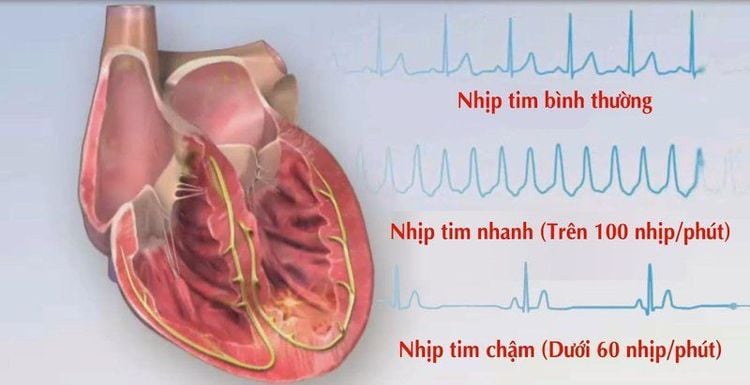
The hemodynamic disturbances that may be encountered during endotracheal anesthesia during endoscopic bladder neck polypectomy are hypertension, hypotension, and cardiac arrhythmias. The treatment will depend on the symptoms and specific causes of each case.
3.3. Complications due to endotracheal intubation
Failure to intubate: can be managed by switching to difficult intubation procedures or switching to another method of anesthesia. Misplaced in the stomach: The endotracheal tube was mistakenly placed in the stomach when listening to the lungs without alveolar murmur, EtCO2 could not be measured. In this case, the doctor will proceed to re-intubate the endotracheal tube. Vocal-tracheal-bronchospasm: When it is difficult or impossible to ventilate the patient, auscultates the lungs with rales or mutes the lungs, the anesthesiology team will handle it by providing adequate oxygen, adding sleeping pills and relaxing muscles, ensure ventilation and give bronchodilators, corticosteroids. If breathing is still not controlled, proceed to a difficult intubation procedure. In addition, some injuries may occur during intubation such as bleeding, broken teeth, damage to the vocal cords, falling foreign objects into the airways,... The doctor will be handled on a case-by-case basis. specific situations.
3.4. Respiratory complications
If the endotracheal tube is folded, retracted, pushed deep into one lung, collapsed or opened the respiratory system, the oxygen source is exhausted, the soda is ineffective, ... will lead to hypoxia and hypercapnia. Anesthesia team will immediately ensure ventilation, oxygen supply and quickly find and treat the cause.

3.5. Complications after extubation
Patients may experience many complications after extubation such as respiratory failure, sore throat hoarseness, laryngotracheal spasm, upper respiratory tract infection, laryngotracheal stenosis, ... The doctor will treat according to the specific symptoms and causes.
To ensure safety as well as limit functional complications after endotracheal anesthesia for laparoscopic bladder polypectomy, patients should strictly follow the doctor's instructions.
Vinmec International General Hospital is one of the hospitals that strictly applies safe surgical anesthesia practice standards according to international guidelines. With a team of experienced anesthesiologists and nurses, along with modern equipment such as nerve detectors, ultrasound machines, Karl Storz difficult airway control system, anesthesia monitoring system GE's comprehensive AoA (Adequate of Anesthesia) including monitoring of anesthesia, pain and muscle relaxation will deliver high quality and safety, helping patients to have adequate anesthesia, not awake, no residual relaxant muscle after surgery. Vinmec Health System is also proud to be the first hospital in Vietnam to sign with the World Anesthesiology Association (WFSA) towards the goal of becoming the safest hospital for surgical anesthesia in Southeast Asia.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.