Vascular pathologies of the spinal cord (Part 2)
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International Hospital.
Knowledge of comorbidities, clinical presentation, and contemporary monitoring techniques can enable a rapid diagnosis of spinal ischemia, when therapeutic therapies can be applied with potential highest probability of success. This section examines the clinical presentation, imaging, and treatment options of this potentially devastating disease.
Part II: Spinal Infarction
1. Epidemiology, risk factors for spinal infarction
Spinal cord infarction is estimated to account for only 1% to 2% of all ischemic strokes and 5% to 8% of all spinal cord diseases. However, spinal ischemia occurs in 4% to 33% of patients with the most obvious risk factor for the disease: thoracic-abdominal aortic surgery.
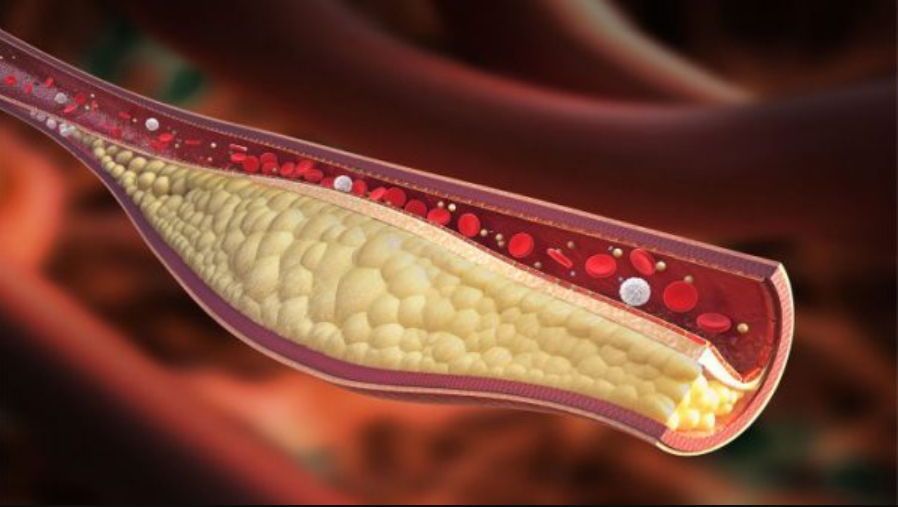
Patients with this particular risk factor include those with extensive surgery between T6 and L2, open surgery, acute aortic dissection, surgery for abdominal aortic aneurysm, advanced age, and other predisposing factors. vascular risk factors, and have atherosclerosis.
The mechanism of ischemia is often multifactorial and involves atherothrombosis, ligation or occlusion of the segmental branches of the aorta, and hypoperfusion due to the commonly used low blood pressure target. to reduce bleeding during surgery.
2. Causes of spinal cord infarction
2.1 Involved in surgery, procedures Aortic surgery Vertebral angiography Extracorporeal membrane oxygenation (ECMO) Intra-aortic balloon counterpulsation Renal artery plug 2.2 Embolization Cardiac thrombosis (eg, atrial fibrillation, endocarditis, paradoxical embolism) Cartilage embolism Decompressive disease Aortic embolism 2.3 Aortic dissection Vertebral artery Subclavian artery 2.4 Vasculitis Blood Syphilis Varicella-zoster virus Systemic vasculitis (eg, polyarteritis nodosa) Primary CNS arteritis 2.5 Atherosclerosis Atherosclerotic segmental occlusion or plaque rupture
Tình trạng xơ vữa động mạnh có thể gây tắc đoạn động mạch
2.6 Systemic hypotension Cardiac arrest 2.7 Vascular malformations Dural arteriovenous fistulas Spinal arteriovenous malformations 2.8 Hypercoagulable state Malignant disease Disseminated intravascular (DIC) rosacea Sickle cell Antiphospholipid antibody syndrome Increased blood homocysteine Retrograde migration of mucinous thrombus fragments from the vertebral vasculature to the radiculo-bulbar arteries is suspected to be the mechanism behind fibrocartilage embolism. . This cause is more common in young adults, in contrast to the peak prevalence of spinal infarction in the 6th and 7th decades of life.
Nodular embolism is caused by physical exertion, trauma, or the Valsalva maneuver and may be responsible for 5% of spinal cord infarctions. Spontaneous myelopathy is a typical condition seen in novice surfers who often have a protracted position with excessive pronation of the thoracic spine and neck for long periods of time.
While the full pathogenesis of this condition is unknown, fibrocartilage embolism is still suspected. Infection or autoimmune vasculitis probably very rarely causes an advanced ischemic myelopathy of the spinal cord, although the disease often affects other organs, and it may also be associated with bleeding manifestations. Despite extensive diagnostic exploration, 20% to 40% of spinal cord infarction cases remain idiopathic.

MRI nhồi máu tủy sống
3. Clinical manifestations of spinal cord infarction
Anterior spinal artery ischemia is the most common. The clinical pattern of ischemia of the posterior spinal artery and the entire spinal cord is likely to be the least common. More than one-third of patients present with unilateral clinical presentation or an unclassified clinical syndrome.
A sudden onset of symptoms is most common in spinal cord infarction, although symptoms may worsen over several hours. Patients with fibrocartilage embolism may develop symptoms several hours after the embolic event.
Perioperative spinal cord infarction occurred intraoperatively in half of the patients, while the other half had late ischemia within 12 to 48 hours of surgery.
Late ischemia in this setting is more common with endovascular techniques and therefore requires close neurologic monitoring after surgery or procedure. Transient ischemic attacks are rare but may herald subsequent true infarction.
Back or neck pain occurs in about one third of patients, is usually radial, may be transient, and is located relative to the level of infarction. The most common focal point with a sensory level is T10. Weakness is initially tender with loss of tendon reflexes, although typical upper motor neuron signs will eventually appear.
However, the upper motor neuron signs may not be evident at the level of medullary injury if there is significant damage to the anterior horn cells of the medulla. While the majority of spinal cord infarctions (65%) occur in the lower thoracic medulla, cervical infarcts are associated with more severe clinical manifestations, including autonomic manifestations and defects in the thoracic region. upper limb.
4. Imaging features of spinal cord infarction
Spinal cord infarction is a clinical diagnosis; however, imaging can be helpful to confirm the diagnosis and rule out other possibilities. CT does not have sufficient resolution to diagnose spinal infarction but may be useful to rule out spinal cord compression due to an epidural hematoma if MRI is contraindicated.
Customers can refer to:
Note that magnetic resonance imaging (MRI) of the brain and spinal cord MRI can show prolonged "pencil-like" T2 signal on longitudinal shear pulses due to toxic spinal edema cell. Contrast enhancement from gadolinium is not usually seen in the acute phase, and the presence of this sign raises suspicion for other causes. Spinal cord atrophy will eventually replace swelling in the chronic phase of the disease.
Signal changes on T2 can take hours to days to manifest, and sensitivity is therefore low during the fulminant phase. In contrast, DWI pulses are capable of identifying fulminant ischemic changes in the spinal cord, but the sensitivity is imperfect because of the small size of the spinal cord and the associated imaging noises.
The overall reported sensitivity of MRI for the diagnosis of spinal cord infarction varies in the literature, and this difference is likely related to the time taken from symptom onset and severity of disease (possibility The ability to capture imaging abnormalities increases with disease severity, and the ability to see signal changes on T2 increases with time).
Furthermore, MRI can give hints about the etiology of the infarction. For example, patients with fibrocartilage embolism often have evidence of disc bulging that corresponds to the site of spinal cord injury. Angiography is not usually indicated in acute spinal infarction unless an arteriovenous fistula is suspected or an unspecified acute aortic dissection is present.
Table: Spinal Vascular Syndromes
Customers can refer to:
Note that magnetic resonance imaging (MRI) of the brain and spinal cord MRI can show prolonged "pencil-like" T2 signal on longitudinal shear pulses due to toxic spinal edema cell. Contrast enhancement from gadolinium is not usually seen in the acute phase, and the presence of this sign raises suspicion for other causes. Spinal cord atrophy will eventually replace swelling in the chronic phase of the disease.
Signal changes on T2 can take hours to days to manifest, and sensitivity is therefore low during the fulminant phase. In contrast, DWI pulses are capable of identifying fulminant ischemic changes in the spinal cord, but the sensitivity is imperfect because of the small size of the spinal cord and the associated imaging noises.
The overall reported sensitivity of MRI for the diagnosis of spinal cord infarction varies in the literature, and this difference is likely related to the time taken from symptom onset and severity of disease (possibility The ability to capture imaging abnormalities increases with disease severity, and the ability to see signal changes on T2 increases with time).
Furthermore, MRI can give hints about the etiology of the infarction. For example, patients with fibrocartilage embolism often have evidence of disc bulging that corresponds to the site of spinal cord injury. Angiography is not usually indicated in acute spinal infarction unless an arteriovenous fistula is suspected or an unspecified acute aortic dissection is present.
Table: Spinal Vascular Syndromes

Các hội chứng mạch máu tủy sống
5. Differential diagnosis of spinal infarction
Pathologies that mimic the clinical presentation of spinal infarction include spinal cord compression secondary to an epidural hematoma, disc herniation, epidural abscess, or malignancy. Other mimics include autoimmune or infectious transverse myelitis, bleeding, or intramyeloma.
If an MRI cannot be performed or is not clear, a cerebrospinal fluid (CSF) test may be necessary. CSF can sometimes be seen to be slightly elevated in protein in spinal cord infarction, but is usually normal.
6. Treatment of spinal cord infarction
The cornerstone of the treatment of spinal ischemia is to improve spinal perfusion by raising blood pressure and reducing CSF jet through CSF drainage. Elevation of blood pressure begins with intravenous fluids immediately followed by vasopressors that are titrated to improve symptoms or adverse events. Placement of a lumbar drain may be considered with an intracranial pressure target of 8 mmHg to 12 mmHg.
Withdrawal from this therapy should be done while closely monitoring neurologic examination to assess for neurologic deterioration over 24 to 48 hours. Although not supported by large trials, clear clinical improvement has been observed in some patients with this approach, so treatment should be tried unless contraindicated.
Intraoperative monitoring with somatosensory and motor evoked potentials, use of iliofemoral conduits, and empiric lumbar drainage can be used concurrently (particularly in high-risk patients) to identify and pave the way for the management of intraoperative spinal ischemia that cannot be seen clinically because the patient is under general anesthesia.
Experience with revascularization with thrombolytics is limited to case reports and is contraindicated in patients with aortic dissection and recent major surgery. Corticosteroids are indicated only for patients with vasculitis.
Currently, there is no evidence to suggest that hypothermia improves outcomes in spinal infarction, although maintaining normal body temperature may reduce secondary neuronal damage. Patients should be monitored for hyperglycemia and hypoglycemia and treated if necessary. Hyperbaric oxygen therapy should be used in patients with spinal cord infarction secondary to decompression sickness.
Patients with high cervical cord injury are at high risk of aspiration due to dysphagia and abdominal muscle weakness leading to weak cough. All patients with spinal infarction should be monitored for concomitant medical problems, including deep vein thrombosis and pulmonary embolism, urinary tract infections, and pressure ulcers.

Điều trị nhồi máu tủy sống cần được thực hiện bởi các bác sĩ chuyên khoa
7. Prognosis of spinal cord infarction
While up to 1⁄4 patients with spinal cord infarction will die, the prognosis for survivors may be better than previously reported. Recovery of neurological deficits can be gradual for many years after infarction.
In one study, 41% of patients in a wheelchair at discharge were able to walk an average of 3 years after discharge, and 1/3 of patients with a bladder catheter at discharge were able to urinate on their own at the first time. the last examination during the follow-up period.
Clinical severity is the strongest and most reliable prognostic marker. Patients with American Spinal Cord Injury Association (ASIA) grades A and B are most likely to have a poor outcome. Bladder dysfunction, somatosensory loss and Babinski's sign, and extensive signal variability on MRI are also associated with poor prognosis.
However, even such patients can improve, especially when modernized methods of rehabilitation are implemented, and this fact should be emphasized for patients and their families. .
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.
Articles refer to the source:
Kramer CL. Vascular Disorders of the Spinal Cord. Continuum (Minneap Minn) 2018;24(2, Spinal Cord Disorders): 407–426.






