Non-culture techniques for the diagnosis of infections in the laboratory - Part 2
Posted by Doctor of Laboratory - Vinmec Central Park International General Hospital
The no-culture technique does not require bacteria to multiply prior to detection. Some techniques, such as microscopy and the detection of bacterial antigens in the specimen. It can provide quick results, for example after 2 hours.
Please follow the article Non-implantation technique to diagnose infections in the laboratory - Part 1
2.10 Radioimmunoassay
Radioimmunoassays can be used to measure antigen concentrations: Binding of radiolabeled antigens is limited to one but standard amounts of antibodies can be partially prevented by the addition unlabelled antigen. The ratio of the free antigen to the limit of antibody that can be used to measure the added unlabelled substance. In practice, it is usually achieved by binding to the antibody from the surface of the plastic pad to facilitate the separation of the restriction from the free antigen.
In another variation, the unlabelled test antigen is added from the homogenization phase antibody and the percentage occupied by the antibody site, which is proportional to the antigen concentration detected by the assay. added a second labeled antibody. This is a trend that now seeks to replace radioisotopes with:
Enzyme markers: like Enzyme link immunosorbent assay (ELISA) the marker in this reaction is an enzyme, this enzyme reacts with the substrate to produce color. The reaction results are observed with the naked eye or read with a spectrometer. Immunofluorescence method: A very sensitive method.

Thử nghiệm miễn dịch huỳnh quang trực tiếp
2.11 Monoclonal antibodies
Monoclonal antibodies can differentiate between species and clones of the same species on the basis of antigenic differences: The principle of the monoclonal antibody technique is to immortalize antibody-producing lymphocytes , and then separate each lymphocyte line by homogenization. Monoclonal antibodies with great utility are increasingly used in immunological techniques that require high sensitivity and specificity such as for the diagnosis of rotaviruses, HIV, hepatitis B, herpes, and syncytial virus. respiratory tract (RSV) can all be directly detected with monoclonal antibodies by ELISA. Chlamydia trachomatis infection can be diagnosed within hours by direct fluorescent antibody testing utilizing a fluorescently labeled monoclonal antibody.
2.12 Detection of bacteria by probing its genes (DNA probe hybridization technique)
Bacteria carrying virulence factors can be detected by nucleic acid probes for virulence factors. Probe a gene that is a specific single-stranded nucleic acid molecule labeled with a radioisotope or enzyme. Hybridization occurs: the DNA probe will find its corresponding DNA fragment in the specimen to recombine to form a double stranded. Having hybrid DNA means that pathogenic bacteria are present in the specimen. Probing the structure of virulence factors such as toxins, bacteria carrying those genes can be detected in patient samples without the need for culture. Example: Escherichia coli enterotoxin or cholera toxin can be detected directly in feces. Commercially available I125-labelled DNA probe directly contacts specific fragment, ribosomal RNA of Mycoplasma pneumoniae successfully used to detect bacteria in sputum specimens.
2.13 Nucleic acid probe
Nucleic acid probes are limited to a small number of bacteria: There is no doubt that gene probes will grow for diagnostic purposes, but it can also detect small numbers of bacteria. (e.g. several copies of a gene) may be constrained by a limiting factor and in that case gene amplification by PCR by hybridization with oligonucleotide probes may become the method of choice, especially for bacteria grow slowly and are difficult to grow in the laboratory.
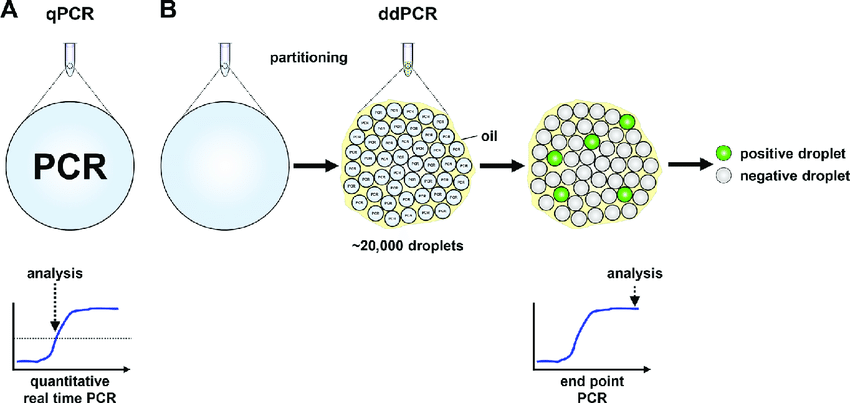
Kỹ thuật PCR trong ứng dụng thăm dò acide nucleic
PCR can reuse a specific piece of DNA to make billions of copies in just a few hours: Although theoretically, PCR can detect a single gene fragment such as susceptibility is rarely achieved in a sample. clinical specimens. But bacteria present in numbers between 10-100 can be detected by standard PCR and more sophisticated methods that can detect pre-HIV DNA fragments in 106 cells. Even more advantageous is the speed with which it still gets results. Amplification takes only about 5 hours, although exploratory or ongoing confirmation of product presence can take more than 36 hours, which should only be accelerated with micro-array techniques.
Specificity of PCR is determined by careful selection of primers: These primers (oligonucleotides) are complete from the target DNA, so in the matching primer sequence, the sequence of the target DNA must be known. . At the moment this is a limitation of PCR, but this multi-use technique will certainly be developed for widespread clinical application. It is currently only used in laboratory research but it appears to be a matter of time before the method can be used in routine diagnosis. Recently, PCR has been applied in various clinical specimens such as cerebrospinal fluid, urine, sputum, blood, biopsies... to the diagnosis of infections caused by bacteria, viruses, fungi and protozoa.
Specificity of PCR is determined by careful selection of primers: These primers (oligonucleotides) are complete from the target DNA, so in the matching primer sequence, the sequence of the target DNA must be known. . At the moment this is a limitation of PCR, but this multi-use technique will certainly be developed for widespread clinical application. It is currently only used in laboratory research but it appears to be a matter of time before the method can be used in routine diagnosis. Recently, PCR has been applied in various clinical specimens such as cerebrospinal fluid, urine, sputum, blood, biopsies... to the diagnosis of infections caused by bacteria, viruses, fungi and protozoa.
2.14 Bacterial culture
Bacteria and fungi can be cultured on solid nutrient medium or liquid medium. Bacteria and fungi grow on the surface of a dense nutrient medium from which colonies of thousands of cells arise from a single cell cultured on the agar surface. The clumps of different species often have a characteristic appearance that can be evidenced from their similarity. It takes 12-48 hours for the colonies of most species to become visible to the naked eye, but some bacteria multiply more slowly and can take several weeks to produce a visible cup. . Inoculation can also be made on liquid medium and growth is detected by observing the turbidity of the medium
However, it cannot be said that more than one species may be present in the inoculum nor is it known How many bacteria are there? Condensed media are useful in bacteriological diagnosis.

Vi khuẩn được cấy trong môi trường đầy đủ dinh dưỡng (bề mặt thạch)
2.15 Different species of bacteria and fungi have different growth requirements
It is possible that most species of medically important bacteria and fungi grow on artificial media in the laboratory, but no single culture medium will demonstrate the growth of all of them. There are still a few species that can only grow in laboratory animals, for example: Mycobacterium leprae and Treponema pallidum . Some bacteria can be grown on artificial media, for example, chlamydia and rickettsia can be grown on cultured cells.
There are many cultures prepared not only to demonstrate the growth of bacteria but also to inhibit the growth of some other bacteria, for example selective media. The medium is important for laboratory diagnostic use and plans to use this medium for the differential conduct of clinical specimens.
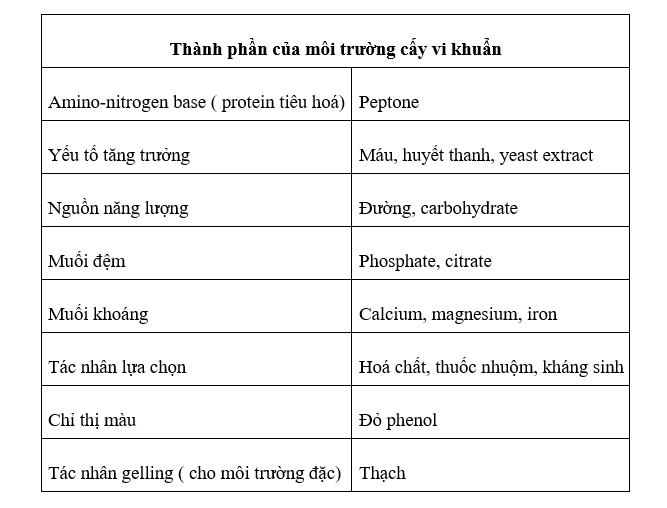
Specimens selected from sites on the body with few resident bacteria will mix with recognized pathogens. Specimens must be carefully collected, nutrient selection and media selected for the production of individual colonies. This is a subculture from a clean medium for identification and susceptibility testing of antibiotics. It takes at least 48 hours and sometimes longer to bring results.
Parasites such as Leishmania, Trypanosoma and Trichomonas can be cultured in a liquid medium allowing small amounts to be present in the initial specimen eg: Blood and vaginal secretions to duplicate and thus become readily available. easily detected by microscopy. Parasites do not form colonies on solid media in the same way as bacteria and fungi.
2.16 Viruses, chlamydia and rickettsia must grow in cells or cultures
Because this bacterium is not able to survive in the free environment. Most of the living cells used in laboratory diagnostics are further line-human or animal cells adapted for in vitro growth that can be stored at -80°C until required. Specimens were introduced in cell culture and the presence of virus was detected by observing cells for cytopathology (CPE).
The cell culture technique is specialized and requires a lot of effort and some viruses that do not cause CPE, eg rubella or cause CPE take 1 week or more to progress sequentially eg cytomegalovirus (CMV); Although CMV antigen is detectable after 1-2 days in cells. Therefore other methods such as antigen or antibody detection are used to diagnose viral infections wherever possible.






