The article was professionally consulted by Dr. Nguyễn Hải Hà - Head of the Vaccine Unit - Faculty of Pediatric Outpatient - Pediatric Center - Vinmec Times City International Hospital.
According to the World Health Organization (WHO), rabies is a widespread disease worldwide. Every year, over 10 million people are bitten by rabid or suspected rabid animals and require post-exposure rabies vaccination. Approximately 60,000 - 70,000 people die from rabies, with most cases reported from tropical countries.
In Vietnam, rabies is prevalent in most provinces/cities. Between 1990 to 1995, the mortality rate was 0.43 per 100,000 people, with an average of 350-500 deaths each year. In 1996, the Prime Minister issued Directive 92 on escalating rabies preventive and control measures. Coordinated preventive measures were established and reinforced, resulting in a 75% reduction in the number of deaths from 1996 to 2007 compared to 1995. In 2007, the entire country recorded 131 deaths, and by 2017, the number had decreased to 74 deaths. Rabies is an extremely dangerous disease when symptoms manifest, with a 100% fatality rate for both the victim and the rabid animal. The incubation period for rabies ranges from a few days to several months, even years, while the time from the onset of symptoms to death only varies from 2 to 10 days.
1. What is rabies?
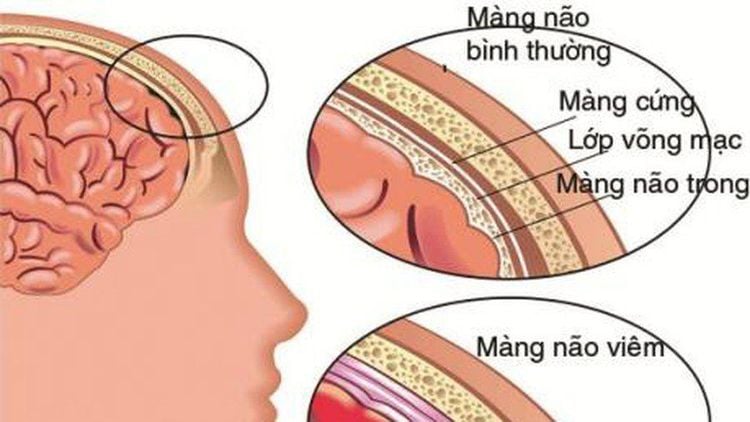
Rabies is an acute viral infection (a RNA virus of the rhabdovirus family) of the central nervous system transmitted from animals to humans through secretions, usually saliva infected with the rabies virus. Most cases of rabies exposure occur through bites or licks from rabid animals. Occasionally, transmission can happen through contact, such as inhaling aerosolized virus or being infected from organ transplants from recently infected individuals. Once symptoms appear, both the animal and the victim will have fatal prognosis with little chance of survival.
- Prodromal phase: usually 1-4 days, characterized by feelings of fear, headache, fever, fatigue, discomfort, and a tingling and painful sensation at the site of infection.
- The encephalitis stage often manifests as insomnia, increased sensitivity to stimuli such as fear of light, fear of water, fear of noise or wind breezes. In addition, there are disturbances in the autonomic nervous system such as pupil dilation, increased salivation, sweating, low blood pressure, and sometimes spontaneous ejaculation. The illness usually lasts from 2 to 6 days, sometimes longer, and eventual death is due to paralysis-induced respiratory failure.
The disease progresses in two basic forms:
- Encephalitic form: This occurs in 80% of rabies patients. The first symptoms are fever, headache, or exhaustion, accompanied by loss of appetite, insomnia, restlessness, and the appearance of symptoms such as hydrophobia and aerophobia. In the progressive stage, the patient experiences increased salivation, making it impossible to chew or swallow, and they frequently spit. After that, the patient's pupils will dilate, causing their eyes to appear bright with streaks, with symptoms of throat spasms, spontaneous ejaculation, priapism, and rapid progression to death.
- Paralytic or "silent" form: Paralysis is a prominent symptom. Symptoms of paralysis appear from the hands and feet to the muscles, causing disturbances in urination and defecation. As soon as the paralysis spreads to the respiratory muscles, the patient will die.
2. The incubation period of rabies in humans
The incubation period for rabies is the time before the onset of symptoms. The period from the time of infection to the appearance of the first symptoms (incubation period) is usually 1 to 3 months in humans. This period is rarely shorter than 9 days or longer than 1 year. However, there are special cases where the incubation period is 4 days and can extend up to 6 years. The incubation period depends on the location and severity of the wound and the amount of virus introduced.
Once symptoms appear, death typically occurs 2-10 days later, with little chance of survival, even with intensive care.
3. Rabies post-exposure prophylaxis in humans
Not 100% of people bitten by animals get rabies. The risk of rabies infection depends on many factors, including whether the animal has rabies or not, the amount of virus in the animal's saliva, the depth of the wound, and whether the wound was cleaned and disinfected promptly after being bitten by the animal... Immediate vaccination post-exposure is still the most effective preventive and protective measure. When bitten, scratched, or licked by an animal on the affected skin area, the following steps should be taken:
3.1. Wound management:
- It is necessary to separate the clothing from the bite, using scissors to cut away the fabric at the bite site (if any). This helps limit the animal's saliva from adhering more to the wound.
- Wash the wound under a strong stream of running water for 15 minutes, warm water is recommended. Then, clean the wound with 70% alcohol, iodine alcohol, or Povidone-Iodine, and absolutely do not attempt to squeeze out the blood. Do not rub the wound, as it may worsen the injury. Do not apply leaves, kerosene, or any substances to the wound.
- After cleaning the wound, the patient should use medical gauze or clean cloth to bandage the wound to stop the bleeding and prevent bacteria from entering. However, do not bandage too tightly as it can obstruct blood circulation. If the wound needs to be stitched to stop the bleeding, it should be stitched loosely, not cosmetically.

3.2. Vaccination for tetanus, rabies, and rabies antiserum:
Patients need to seek medical intervention immediately to receive tetanus vaccine, rabies vaccine, and rabies antiserum (if the wound is grade III) right after being bitten by a rabid animal. The vaccination schedule and type of rabies vaccine will be advised by doctors according to the wound classification and post-exposure prophylaxis treatment protocol.
Post-exposure rabies vaccination will have two regimens: intramuscular injection and intradermal injection.
Intramuscular injection is used in rabies vaccination schedule when exposure has been confirmed (already bitten):
- For those who have not been vaccinated before exposure: 5 doses (0.5ml/dose) on days 0, 3, 7, 14, 28. In the case of level III exposure, it is necessary to combine it with rabies immune globulin injection.
- People who have been vaccinated in the past 5 years: Administer 2 doses on days 0 and 3.
- People who have had irregular or more than 5 years since the last vaccination: Administer 5 doses on days 0, 3, 7, 14, 28 and may also receive rabies immune globulin.
- Intradermal injection is used in rabies vaccination schedule at dosage of 0.1ml x 2:
- People who have not been vaccinated before exposure: Inject 4 doses: inject at different sites on both limbs, each side with a dosage of 0.1 ml, on days 0, 3, 7, and 28.
- For those who have received prophylaxis: Inject 0.1ml on days 0 and 3.
To arrange an appointment, please call … or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.








