This is an automatically translated article.
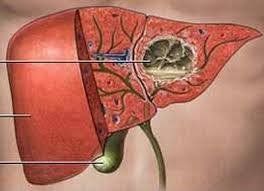
Liver abscess is a collection of pus in the liver caused by an amoeba, bacterial or fungal infection. From there, it causes symptoms such as fever, enlarged liver, right lower quadrant pain... So why is liver abscess common in the right lobe? How is this disease diagnosed and treated?
1. Why is liver abscess common in the right lobe?
1.1. Pathogenesis Before answering this question, it is important to know about the pathways by which pathogens can reach the liver:
Biliary system: Diseases of the biliary tract such as cholecystitis, cholangitis , common bile duct stones , worms in the bile ducts ... can lead to liver abscess . Pathogens from inflammatory foci in the biliary tract, or in bile, from obstruction of the bile duct can regurgitate into the intrahepatic bile duct, where they begin to form pus-abscesses. Portal vein: Pathogens can be absorbed from the intestinal tract, or other abdominal organs, into the superior mesenteric vein, inferior mesenteric vein, superior rectal vein, The splenic vein, and the coronary vein, are concentrated in the portal vein and travel to the liver. Hepatic arteries and systemic lymphatics: In some patients, there is bacteremia, systemic infection or in organs such as lungs, kidneys, meninges, urinary tract, lymph nodes... Diseases from infectious foci inside and outside the liver will follow the lymphatic route or hepatic artery to the liver and form pus-filled abscesses. 1.2. Causes of right lobe liver abscess more often than left lobe According to research reports on the rate of people with liver abscess, liver abscess involving the right lobe accounts for about 75% of cases, while the left lobe accounts for only 20 % and the rate of liver abscess in both lobes was 5%.
According to the ways in which pathogens are amoeba and bacteria can come to cause disease, this ratio can be explained as follows:
Structure of the liver: According to the lobe division, the liver is divided into 2 lobes left and right with 5 lobes anterior, posterior, lateral, middle and dorsal. In which, the anterior, posterior and middle lobes belong to the middle lobe and the lateral segment belongs to the left lobe, and the dorsal segment belongs to the caudal lobe. This division shows that the area and volume of the right lobe is 2 or 3 times larger than that of the left lobe. Therefore, structures such as the biliary system, portal vein, artery and lymphatic system in the right lobe will be larger and more numerous than in the left lobe. This also explains that the right lobe of the liver is responsible for most of the liver's functions. Biliary system: In the liver, the bile duct is divided into many ducts for each subsegment and segment. Specifically, the right hepatic duct is the convergence of the subsegments VI, VII of the posterior segment, and the subsegment V and VIII of the anterior segment of the right lobe of the liver. The left hepatic duct is the convergence of the lateral segment II and III subsegmental ducts (left lobe of the liver) and the middle segmental ducts (right lobe of the liver). At the same time, the length of the right hepatic duct (9 cm) is usually shorter than that of the left hepatic duct (15-20 cm). With such anatomical structure, when there is an infection upstream from the biliary tract to the liver, the risk of exposure to pathogens of the right lobe will be higher than that of the left lobe. Portal vein system: The portal vein receives blood from the superior mesenteric vein, inferior mesenteric vein, gallbladder vein, left gastric vein, right gastric vein, prepyloric vein, and other veins side of the navel then drains to the liver. When approaching the liver, the portal vein turns right and divides into two main branches, the right branch drains into the right lobe and the left branch drains into the left lobe. The right branch receives about 75 - 80% of the blood volume to the liver, while the left branch receives about 20 - 25% of the blood volume, but mainly from the splenic vein, umbilical vein and ductus venosus. At the same time, in terms of structure, the right branch of the portal vein is usually larger, straighter and shorter than the left branch. Due to the large volume of blood flowing to the liver along with the anatomical structure of the right branch of the portal vein, the right lobe of the liver will have a higher risk of exposure to pathogens than the left lobe. Hepatic and lymphatic arteries: The right lobe of the liver includes the anterior, posterior, and middle lobes, respectively, receiving blood from the anterior, posterior and middle lobe arteries, accounting for about 70 - 80% of the blood supply to the liver. In contrast, the left lobe of the liver receives blood from the lateral segmental artery, which accounts for about 20 to 30 percent of the blood supply to the liver. At the same time, with a larger area than the left lobe, the right lobe of the liver has a larger lymphatic system than the left lobe. Therefore, the proportion of pathogens from extrahepatic foci of infection entering the right lobe will be greater than the left lobe.
2. Clinical symptoms of liver abscess
2.1. Amoebic liver abscess Fontan's triad includes fever, right upper quadrant pain, hepatomegaly, and tenderness of the liver. Other less common symptoms include jaundice, pericardial rub, and peritonitis. 2.2. Bacterial liver abscess Right upper quadrant pain. High fever can reach 39-40 degrees Celsius, chills. The liver may be enlarged and painful on examination by intercostal compression. Weight loss, jaundice, loss of appetite, fatigue, loose stools.
3. Diagnosis of liver abscess
3.1. Amoeba liver abscess Blood count: WBC may be elevated. Biochemistry: CRP increased. Coagulation tests: Increased sedimentation time. Serology: The ELISA reaction has high sensitivity and specificity. Ultrasound: The lesion is hypoechoic, well demarcated, round or oval, single or multifocal. Chest X-ray: Right diaphragm is pushed up, right pleural effusion may be present. Abdominal computed tomography (CT - scan): Helps diagnose the location of the abscess and differentiate it from other lesions such as liver cancer. Aspiration of abscess: Aspiration of chocolate color, odorless, pus culture without bacteria, sometimes find amoeba in the pus. 3.2. Bacterial liver abscess Blood count: WBC increased, mainly neutrophils. Coagulation tests: Increased sedimentation time. Blood biochemistry: CRP increased, Procalcitonin increased. Aspiration of abscess, culture of pus, blood culture for antibiotic chart: Bacteria can be found. Imaging: Ultrasound will show a hypoechoic mass or mixed echo. CT scan of the abdomen helps to diagnose the location of the abscess and distinguish it from other lesions in the liver.
4. Treatment of liver abscess
4.1. Medical treatment of Amebic liver abscess
First choice: Metronidazole 750 mg orally 3 times a day or 500 mg intravenously every 6 hours, treatment duration 10-14 days. Or Tinidazole orally 2 g per day, duration of treatment 3 days. Accompanied with Diloxanide furoate 500 mg orally 3 times daily for 10 days or Paromomycin 10 mg/kg orally 3 times daily for 7 days. Alternative medicine: Start with Emetine or Dehydroemetine 1 mg/kg subcutaneously or intramuscularly daily, treatment duration 8-10 days. Then use Chloroquine 500 mg orally twice daily for the next 2 days and then 500 mg orally every day for the following 21 days. Accompanied with Diloxanide furoate 500 mg orally 3 times daily for 10 days or Paromomycin 10 mg/kg orally 3 times daily for 7 days. Amoebic drugs in the form of cocoon in the intestine: Oral Intetrix inflammatory form, for 7-10 days. Add antibiotics if there is a bacterial superinfection. Bacterial liver abscess
First-line antibiotic choice: Choose penicillin group of antibiotics combined with Beta Lactamase inhibitor group such as Ampicillin - sulbactam intravenous infusion (TTM) 1.5 - 3 g/6 hours. Group of 3rd or 4th generation Cephalosporins such as Ceftriaxone IV 2 – 4 g/time/day or Ceftazidime IV 1 – 2 g/time every 12 hours or Cefepim IV 1 – 2 g/time every 12 hours. Combined with Metronidazol TTM 500 mg/8 hours if the antibiotic chart has anaerobic bacteria infection. Alternative antibiotic options: Quinolones such as Ciprofloxacin 500 mg orally or IV every 12 hours. Or Levofloxacin 500 mg orally or IV every 12 hours. Combined with Metronidazol TTM 500 mg/8 hours if the antibiotic chart has anaerobic bacteria infection. In case patients have severe symptoms or patients do not respond to other antibiotics above: Use Carbapenem group such as Meropenem IV 1 g every 8 hours or Imipenem - Cilastatin IV 1 - 2 g every 12 hours or Doripenem IV 0, 5 g every 8 hours. The duration of treatment for bacterial liver abscess ranges from 2 to 4 weeks, depending on the patient's response. 4.2. Aspiration and drainage of the abscess Aspirate the abscess in the following cases:
Uncertain diagnosis Large abscess with a diameter of ≥ 5 cm. Patients do not respond after 3-5 days of treatment. Risk of rupture of liver abscess. Risk of rupture of left lobe liver abscess spilling into the pericardium. Patients diagnosed late > 3 months. Patients with indications for aspiration and drainage of the abscess must still be treated with drugs.
The division of the liver lobe along with related anatomical structures such as the portal vein system, arteries, lymphatics and intrahepatic biliary tract makes the right lobe liver abscess occur more often than the lobe liver abscess. left. Detecting symptoms and early diagnosis, and applying appropriate treatment methods will help patients and their loved ones improve the effectiveness of treatment, and at the same time limit the complications of liver abscess. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.