This is an automatically translated article.
The article is professionally consulted by Master, Doctor Dang Xuan Cuong - Emergency Resuscitation Department - Vinmec Hai Phong International General Hospital. The doctor has 14 years of experience in the field of emergency resuscitation and poison control.The pancreas is an important organ of the human digestive system. So what is the function of pancreatic juice secreted from the pancreas, let's find out through the article below.
1. General overview of pancreas and pancreatic juice
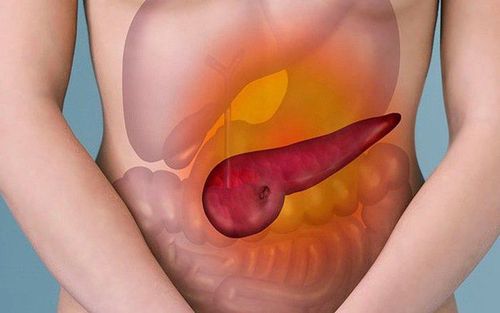
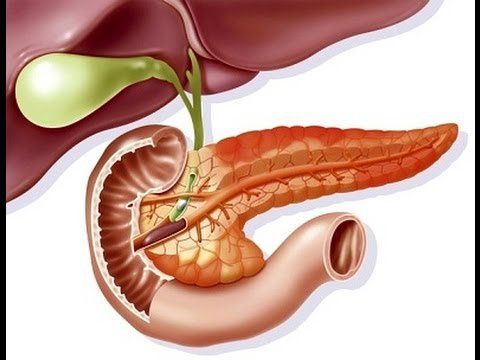
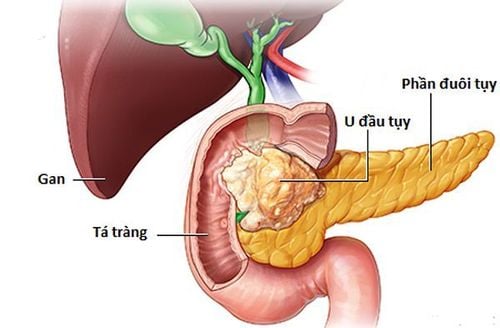
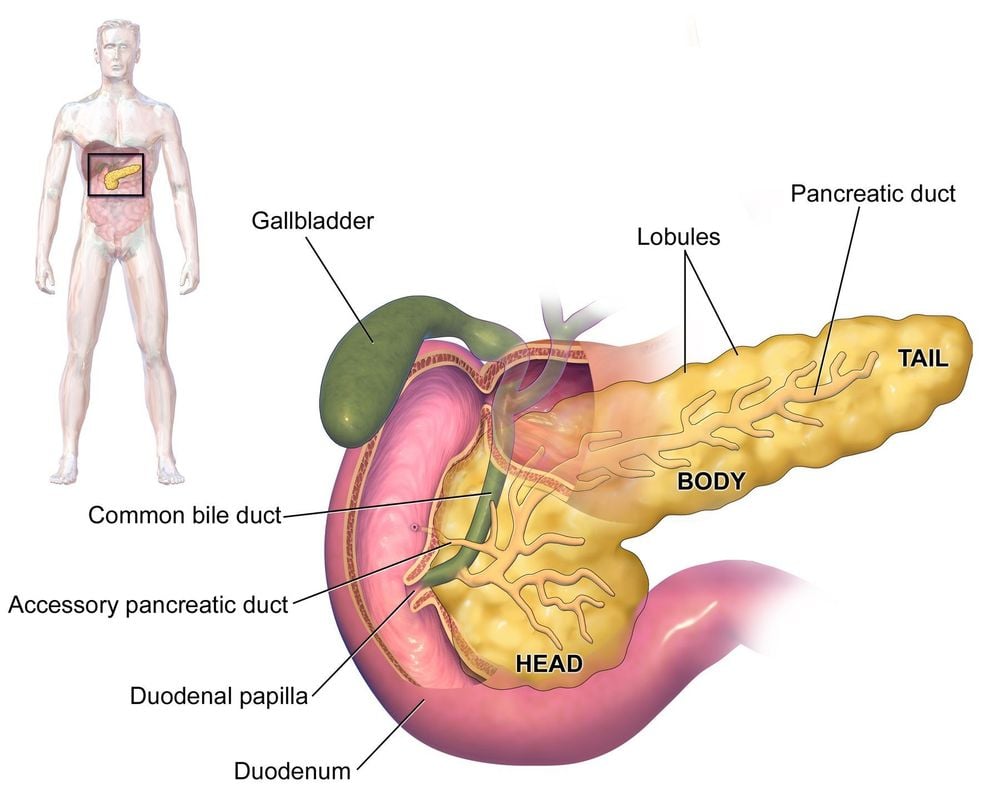
The pancreas is an organ of the body, located in front of the posterior abdominal wall, an organ behind the peritoneal cavity. The pancreas is about 15cm long, 6cm high, 3cm thick, located across the spine, starting from the duodenum and ending at the armpit.The pancreas weighs about 80g, the soft tissue of the pancreas is pale white. The structure of the pancreas consists of 5 parts: the pancreatic apex, the head of the pancreas, the neck of the pancreas, the body of the pancreas and the tail of the pancreas (the tail of the pancreas is the only part of the pancreas that is located in the junction of the spleen and kidney, between the two peritoneal leaves).
The pancreas is a special organ that has both an exocrine function (secreting pancreatic juice). What is the function of pancreatic juice? It has the ability to digest almost all ingredients in food), and has an endocrine function (secreting hormones, typically insulin).
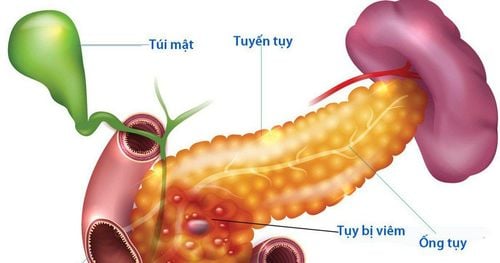
Pancreatic juice is led out into the digestive tract through two pancreatic ducts, the main pancreatic duct and the accessory pancreatic duct. The main pancreatic duct (Wirsung's duct) runs the length of the pancreas, joins the common bile duct to form the ampulla of Vater before emptying into the second segment of the duodenum, and the sphincter of Oddi surrounding the foramen is responsible for regulating bile flow. and pancreatic juice into the duodenum. The accessory pancreatic duct (santorini) collects pancreatic juice from the apex and head of the pancreas and pours it into the accessory pancreatic foramen slightly above the ampulla of Vater. In the pancreas, the main pancreatic duct and the accessory pancreatic duct are connected.
Tuyến tụy vừa có chức năng ngoại tiết vừa có chức năng nội tiết
2. Composition and function of pancreatic juice
Approximately 1000 mL of pancreatic juice is secreted per day, in which the pancreatic cysts secrete digestive enzymes, and the ducts that drain from the cysts excrete bicarbonate salts.Pancreatic juice has all 3 enzymes to digest almost all components found in human food (carbohydrates, proteins, lipids). Most enzymes are produced and excreted as inactive pro-enzymes (except amylase and lipase) encased in zymogen granules. These pro-enzymes are converted to the active form when exposed to an enzyme in the brush border of the intestinal cells called enterokinase.
Specific digestive enzymes include:
To digest carbohydrates: The enzymes amylase, maltase will hydrolyze polysaccharides (except cellulose), oligosaccharides, trisaccharides (maltotriose) and disaccharides (maltose) to finally produce monosaccharides which are glucose. For protein digestion: The pancreas secretes pro-enzymes (trypsinogen, chymotrypsinogen, procarboxypeptidase, ribonuclease, deoxyribonuclease, proelastase), when emptying into the duodenum to meet enterokinase, trypsinogen converts to the active form trypsin, which activates the remaining pro-enzymes. into the active form chymotrypsin, carboxypeptidase, ribonuclease, deoxyribonuclease, elastase to hydrolyze proteins into short peptide chains, and then undergo contact with other enzymes in the intestine to become amino acids that the intestines can absorb collect. However, an enzyme called carboxypeptidase is capable of severing peptide bonds with a terminal -COOH radical to form single amino acids that can be absorbed by the intestines. For lipid digestion: Lipid-digesting enzymes are water-soluble compounds that can only be broken down on the surface of lipid particles, for that reason, in order to digest lipids, the first step is that the lipids need to be emulsified. metabolized by bile. Bile salts and lecithin in bile play a role in reducing the surface tension of lipid granules, and when the surface tension is reduced, intestinal contractions will break the lipid granules, creating smaller particles, making the surface surface smooth. The contact surface between the enzyme and the particles increases up to 1000 times. The lipase enzyme hydrolyzes the emulsified lipid particles to triglycerides and then to fatty acids and monoglycerides. Cholesterol ester hydrolase reacts with cholesterol ester to form cholesterol and fatty acids. And phospholipase A2 reacts with lecithin to produce lysolecithin. In addition, bicarbonate ions (in bicarbonate salts) are extremely important components that play a role in neutralizing acid from the stomach to the duodenum.
An interesting point is that the pancreas has a defense mechanism to protect itself from being affected by the digestive juices it secretes, namely:
Most enzymes are in the precursor form and only occur when they are reduced to the small intestine. Digestive enzymes are encased in zymogen granules of follicular cells. Follicular cells synthesize and secrete trypsin inhibitors, which counteract premature activation of trypsinogen, because trypsin activates other protein-digesting enzymes as well as phospholipase A2. If phospholipase A2 is activated in the pancreas, it causes cell damage, disrupting pancreatic tissue and destroying surrounding fatty tissue.
Dịch tụy được điều hòa bài tiết theo hai cơ chế là thần kinh và nội tiết
First stage: When looking, smelling, thinking about food or chewing and swallowing food, The X nerve will secrete acetylcholine to secrete enzymes into the pancreatic cyst, and during this period, pancreatic juice contains many enzymes, and pancreatic juice accounts for 20% of the gastric juice of the entire meal. Gastric phase: When the stomach is distended, it activates the long reflex arc of the X nerve - the X nerve. Acetylcholine secreted by the X nerve will stimulate both pancreatic follicular cells and pancreatic ductal cells, although However, the amount of enzyme secreted will be more than the amount of bicarbonate. At this time, gastric juice usually accounts for only 5-10%. Intestinal stage: In this stage, gastric secretion is abundant, up to 70-80%. When responding to secretin and cholecystokinin, the pancreas will secrete a lot, specifically as follows:
When the concentration of H + ions is high in the duodenum, it will stimulate the S cells in the duodenum as well as in the first part of the jejunum to release secretin stimulates the ducts to secrete bicarbonate ions, and secretin also stimulates the liver to excrete bicarbonate. A variety of fatty acids, amino acids, and peptides stimulate the I cells of the duodenum and jejunum to release cholecystokinin into the bloodstream, which then stimulates the pancreatic cyst to secrete digestive enzymes. H + ions, fatty acids and peptides also play a role in stimulating the secretion of pancreatic juice, especially enzymes through the long reflex arc of the X - X nerve.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article reference source: webmd.com