This is an automatically translated article.
Article by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Colitis is an inflammation of the entire colon. Generalized colitis is most commonly caused by ulcerative colitis (UC), which can also be caused by a C. difficile infection, or by inflammatory disorders such as rheumatoid arthritis (RA).
1. Overview
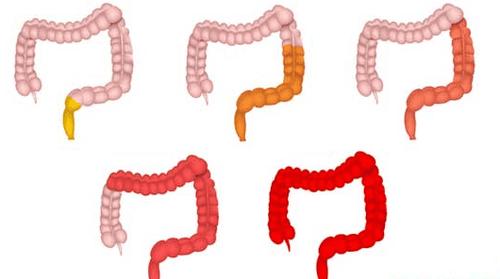
Ulcerative colitis is a chronic condition affecting the lining of the large intestine or colon, due to inflammation that leads to ulcers or sores in the colon. In total colitis, the inflammation and ulceration have spread to cover the entire colon.
Other types of ulcerative colitis include:
Proctosigmoiditis, in which your rectum and part of your pelvic colon called the sigmoid colon become inflamed and ulcerated. Proctitis, proctitis, affects only your rectum Left-sided, or distal, ulcerative colitis, in which inflammation extends from your rectum to a curve of your colon near your spleen, on the left side of body. Ulcerative colitis causes symptoms that can be uncomfortable or painful. The more colon sites are affected, the worse your symptoms will often be. Because pancreatitis affects your entire colon, its symptoms may be worse than those of other forms of ulcerative colitis.
2. Symptoms of pancreatitis
Common mild and moderate symptoms of total colitis include:
Feeling exhausted Unusual weight loss (not exercising or dieting more) Pain and cramping in the abdomen and your abdomen A strong, frequent, but not always controlled, urge to have a bowel movement As pancreatitis gets worse, severe symptoms are likely more like:
Pain and bleeding from the rectum and anus area Fever of unknown cause Bloody diarrhea Purulent diarrhea Some of these symptoms may not necessarily be the result of systemic inflammatory bowel disease. Pain, cramps, and a strong need to expel waste can be caused by bloating, gas, or food poisoning. In these cases, the symptoms resolve after a short period of discomfort.
But if you have the following symptoms, you should see a doctor immediately:
Bloody or pus-filled diarrhea Fever Diarrhea that lasts more than two days that doesn't respond to medicine Passes many loose stools in 24 hours Severe pain flushing in the abdomen or rectum

3. Causes of pancreatitis
It is not known exactly what causes pancreatitis or other forms of ulcerative colitis. As with other inflammatory bowel diseases (IBDs), total colitis can be caused by your genes. One theory is that the genes thought to cause Crohn's disease, another type of IBD, may also cause ulcerative colitis.
The Crohn's & Colitis Foundation of America notes that there is research into how genetics can cause ulcerative colitis and other IBDs. This study includes how genes interact with bacteria in the digestive tract. It is thought that the immune system may mistakenly target the colon while attacking bacteria or viruses that cause infections in the colon. This can cause inflammation and damage to the colon, which can lead to ulcers. It can also make it harder for the body to absorb certain nutrients.
The environment can play a role. Taking certain medications, such as nonsteroidal anti-inflammatory drugs or antibiotics, may increase the risk. A high-fat diet can also be a factor.
In some cases, if a person is left untreated for mild or moderate forms of ulcerative colitis, the condition can get worse and become a case of total colitis.
Some people believe that stress and anxiety can lead to ulcerative colitis and inflammation of the entire colon. Stress and anxiety can trigger sores and cause pain and discomfort, but these factors don't actually cause diverticulitis or other IBD.
4. Diagnosis of pancreatitis
The doctor may want to do a physical exam to get an idea of the patient's overall health. They may then order a stool sample or blood test to rule out other causes of your symptoms, such as a bacterial or viral infection.
The doctor may ask the patient to perform an endoscopy. During this procedure, the doctor inserts a long, thin tube with a light and camera at the end into the anus, rectum, and colon to examine the lining of the large intestine for ulcers and any other abnormal tissue. .
During the colonoscopy, the doctor may take a sample of tissue from the colon to check for any other infections or diseases. This is called a biopsy.
Endoscopy helps the doctor find and remove any polyps that may be present in the colon. A tissue sample and polyp removal may be needed if your doctor believes the tissue in your colon may be cancerous.

5. Treatment of inflammation of the whole colon
Treatments for pancreatitis and other forms of ulcerative colitis depend on the severity of the ulcer in your colon. Treatment may also be different if you have any underlying medical conditions that are causing your pancreatitis or if untreated pancreatitis has caused a more serious condition.
Drug treatment
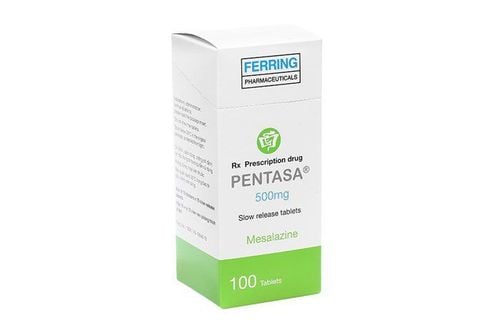
The most common treatments for pancreatitis and other forms of ulcerative colitis are anti-inflammatory medications. These include medications such as oral 5-aminosalicylate (5-ASA) and corticosteroids.
Prednisone can be given, either as an injection or as a rectal suppository. These types of treatment can have side effects, including:
Nausea Heartburn Increased risk of diabetes Increased risk of high blood pressure Osteoporosis Weight gain Medicines that suppress the immune system are also treatments common for pancreatitis and ulcerative colitis. These substances help keep your immune system from attacking the colon to reduce inflammation. Medicines that suppress the immune system for pancreatitis include:
Azathioprine (Imuran) Adalimumab (Humira) Vedolizumab (Entyvio) Tofacitnib (Xeljanz) They can have serious side effects, such as infection. infection and increased cancer risk. You may also need to follow up with your doctor regularly to make sure that the treatment is working.
Surgery
In very severe cases, the surgeon may remove the patient's colon. The surgeon will create a new route for waste in the body to exit the body.
Surgery is usually a last resort. Most people develop ulcerative colitis through a combination of lifestyle changes and medication that can provide significant symptom relief.
Lifestyle changes
Lifestyle changes can help reduce the symptoms of total colitis, avoid pathogens and ensure the body is getting enough nutrients
Foods to avoid:
Eat less more milk. Avoid carbonated drinks. Reduce the amount of insoluble fiber. Avoid beverages that contain caffeine such as coffee and alcohol. Drink plenty of water every day Take a multivitamin. Conclusion
There is no cure for any form of ulcerative colitis other than surgery to remove the colon. Pancreatitis and other forms of ulcerative colitis are chronic conditions, although most people experience high and low levels of symptoms.
Flare-ups in pancolitis can be more severe than in other forms of ulcerative colitis, because more of the colon is affected than in pan-colitis.
If ulcerative colitis is left untreated, potential complications include:
Colorectal cancer Gastrointestinal perforation or a hole in the colon Megacolon – toxic megacolon May improve symptoms and reduce complications by following a treatment plan, avoiding triggers, and seeing your doctor regularly.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Langan RC, et al. (2007). Ulcerative colitis: diagnosis and treatment. aafp.org/afp/2007/1101/p1323.html Mayo Clinic Staff. (2014). Colonoscopy. mayoclinic.org/tests-procedures/colonoscopy/basics/definition/prc-20013624 Mayo Clinic Staff. (2014). Crohn's disease. mayoclinic.org/diseases-conditions/crohns-disease/basics/definition/con-20032061 Mayo Clinic Staff. (2014). Ulcerative colitis. mayoclinic.org/diseases-conditions/ulcerative-colitis/basics/definition/con-20043763 Mayo Clinic Staff. (2015). Inflammatory bowel disease. mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/basics/definition/con-20034908 Ulcerative colitis. (2014). niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis Ulcerative colitis: treatment. (2016). nhs.uk/Conditions/Ulcerative-colitis/Pages/Treatment.aspx