This is an automatically translated article.
Nonspecific bronchopneumonia is a group of idiopathic interstitial pneumonia. This is chronic interstitial pneumonia with a uniform appearance of interstitial inflammation and fibrosis. The name interstitial pneumonia is “nonspecific” because it lacks typical histopathological features. The disease usually involves bilateral lung parenchyma and may have a predisposition to the lower lobes.
1. What is nonspecific bronchitis?
Nonspecific bronchopneumonia is the 2nd most common form and pathology of interstitial lung diseases. The disease has 2 main subtypes:
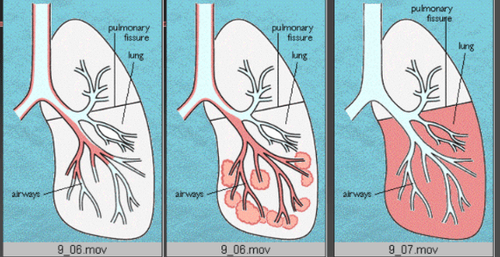
Fibrous type nonspecific interstitial pneumonia: Most common, with a worse prognosis. Cell type nonspecific interstitial pneumonia: Less common, but has a much better prognosis due to a very good response to treatment. On imaging, the most common features of nonspecific interstitial pneumonia are relatively symmetrical and bilateral background glass opacity with associated fine meshes and reduced lung volume, leading to force-induced bronchiectasis. pulled in during respiration.
2. What is the cause of nonspecific bronchopneumonia?
Nonspecific bronchopneumonia whose etiology may be idiopathic or associated with connective tissue disease, HIV infection, toxins, or many other causes. Secondary causes of interstitial pneumonia include:
Connective tissue disease: Interstitial cell pneumonitis is a common form of underlying connective tissue disease, including systemic sclerosis, polymyositis/inflammation dermatomyositis, rheumatoid arthritis and Sjogren's syndrome. Drug-induced: Amiodarone, methotrexate, nitrofurantoin, chemotherapeutic agents and statin therapy. HIV infection: Interstitial pneumonia is less common now than in the past following the widespread use of antiretroviral therapy. Interstitial Pneumonia with Autoimmune Features: These patients have evidence of interstitial pneumonia on lung biopsies and features of autoimmune disease that do not match the specific connective tissue disease. Hypersensitivity Pneumonia: In some patients, lung biopsies lacked granulomas, and histopathologically multinucleated giant cells showed the appearance of interstitial cell pneumonia. Other diseases: Such as IgG4-associated systemic disease, familial interstitial pneumonia, and graft-versus-host disease
3. What are the manifestations of non-specific interstitial pneumonia?
The most common symptoms of patients with nonspecific interstitial pneumonia are dyspnea and a cough that progresses over weeks to months. In addition, sick people may also have fever, weight loss, and flu-like symptoms. If systemic disease is present, the patient may experience dry mouth, dry eyes, arthralgia, joint swelling, muscle pain, dysphagia, skin changes, or other features.
When clinical assessment is needed, patients should be asked about exposure to airborne antigens, a list of medications being taken, history of radiation exposure, HIV risk factors, symptoms associated disease as well as family history.
For the diagnosis of nonspecific interstitial pneumonia, laboratory tests should be performed with an appropriate serological assessment. In addition, HIV testing should also be considered if risk factors are present.
On imaging studies, chest X-ray may show increased baseline findings and/or bilateral interstitial eminence in nonspecific interstitial pneumonia. Nevertheless, high-resolution computed tomography of the thorax is the gold standard for imaging nonspecific interstitial pneumonia. Most common findings may include increased reticular sign, traction bronchiectasis, hypovolemia, and predominant infiltrates in the lower regions.
In addition, lung biopsy may assist in a definitive diagnosis, although it may not always be necessary. The requirement for a biopsy must be assessed in the clinical setting, including whether the underlying procedure is identified, and the severity of the lung injury. For example, in the case of a patient with suspected drug-induced nonspecific interstitial pneumonia, biopsy intervention may not be necessary. Conversely, in cases where no relevant etiology is found, the patient may need a lung biopsy to make a diagnosis.
4. How is non-specific interstitial pneumonia treated?
Treatment of nonspecific interstitial pneumonia depends on the cause and severity of the disease:
Mild disease: These patients usually have mild symptoms and minimal impairment in functional tests lung. At this point, the patient may simply need to be monitored for evidence of disease progression. Moderate to Severe Disease: These patients have moderate to severe symptoms, with significant deterioration on lung function tests as well as diffuse changes on computed tomography. In this case, systemic steroid therapy (prednisone) is usually initiated at 0.5 to 1 mg/kg ideal body weight up to a maximum dose of 60 mg daily for 1 month, followed by 30 to 40 mg daily for an additional 2 months. For those who respond and are stable to this treatment, prednisone should be tapered over 6 to 9 months to a dose of 5 to 10 mg daily or every other day with the goal of being able to stop treatment at 1 year. Typically, patients are monitored for 3 to 6 months of prednisone treatment to assess response to treatment and tolerability before considering a second immunosuppressive agent such as azathioprine or mycophenolate. However, for patients with more severe initial disease, clinicians may initiate systemic steroid therapy along with a second immunosuppressant together. More serious illness that may require hospitalization: These patients may require an initial dose of 1000mg daily for 3 days of methylprednisolone, followed by systemic prednisone therapy as outlined above. Resistant disease despite systemic steroids and immunosuppressive agents: The use of cyclophosphamide inhibitors, rituximab, or calcineurin may be considered. Those who do not respond may be considered for lung transplantation. It is important during treatment to be aware of the possible side effects of steroid therapy and to continue to assess the risks and benefits of steroid therapy. Furthermore, Pneumocystis jiroveci pneumonia prophylaxis should also be considered in patients receiving more than 20 mg of prednisone daily for more than 1 month, or in patients taking multiple immunosuppressants, because of the infection. This can significantly worsen lung function.
In cases where interstitial pneumonia is attributable, the patient should be treated for secondary causes:
Drug cause: May be sufficient to remove from exposure. Connective tissue disease: Treatment focuses on the underlying cause. Collaboration with a rheumatologist may also be helpful. HIV infection: Rule out infections and then initiate antiretroviral therapy. Systemic steroids may be used for those who do not improve. In summary, interstitial pneumonia is a group of idiopathic interstitial pneumonia. This is chronic interstitial pneumonia with a uniform appearance of interstitial inflammation and fibrosis. The treatment of this group of patients is often complex and requires close follow-up, and emphasizes the role of the inter-specialist team in long-term management and improved prognosis in the future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.