This is an automatically translated article.
We sometimes hear in the media about a terrifying bacterium called a flesh-eating bacterium. So what is man-eating bacteria, is it really "cannibal" or not, let's find out through the article below.1. What is flesh-eating bacteria?
In fact, there are no literal flesh-eating bacteria, but the phrase "flesh-eating bacteria" often used in the media are essentially bacteria that cause necrotizing fasciitis (necrotizing fasciitis - NF).
Necrotizing fasciitis is an uncommon, rapidly progressive, deep subcutaneous infection caused by bacterial toxins that cause inflammation and destruction of connective tissue, fatty tissue, and muscle tissue. The bacteria that most commonly cause necrotizing fasciitis is group A beta hemolytic streptococcal (GABHS). There are also many other bacteria that cause necrotizing fasciitis, such as Vibrio vulnificus, Staphylococcus aureus (Staphylococcus aureus), Klebsiella, Clostridium (Clostridium perfringens, Clostridium septicum,...), E. coli, Aeromonas hydrophila ,...
Necrotizing fasciitis is usually classified into two types. Necrotizing fasciitis type I is caused by a mixed infection (infection with many bacteria), usually a combination of an anaerobic species with one or more facultative anaerobes. Necrotizing fasciitis type II is caused by group A beta-hemolytic streptococcal infection, and between the two types of necrotizing fasciitis, type II necrotizing fasciitis accounts for the majority of cases.

Hình ảnh viêm cân mạc hoại tử ở chân người bệnh
Every year in the United States, about 600 to 700 cases of necrotizing fasciitis are diagnosed, with a mortality rate of 25% to 30%. Necrotizing fasciitis rarely occurs in children.
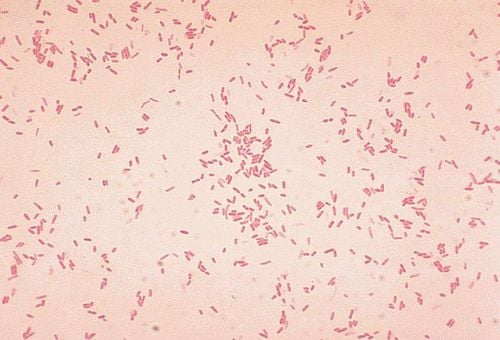
1.1 Group A beta hemolytic streptococcal (GABHS) Group A beta hemolytic streptococci are gram-positive bacteria, in culture they stand in pairs or chain with each other. different lengths. On sheep blood agar culture, colonies of group A beta-hemolytic streptococci are round, small, transparent to opaque clusters, surrounded by an area of completely destroyed red blood cells.
1.2 Vibrio vulnificus Vibrio vulnificus is a motile gram-negative bacterium. Vibrio vulnificus is one of the species of Vibrio (there are about 12 species of human pathogenic Vibrio, the most familiar being Vibrio cholerae and Vibrio parahaemolyticus causing acute gastrointestinal infections with severe diarrhea), belonging to the family Vibrionaceae.
Vibrio vulnificus is commonly found in warm waters and grows well when water temperatures reach above 200C. Vibrio vulnificus was not associated with contamination.
1.3 Staphylococcus aureus is a gram-positive, facultative anaerobic bacterium in the family Staphylococcaceae. In agar, staphylococcus aureus colonies are round, smooth, and appear dark yellow, orange or white after 24 h.

Hình ảnh tụ cầu vàng (Staphylococcus aureus)
2. Path of infection with flesh-eating bacteria
Man-eating bacteria most often enter the body through open wounds, but it can also enter through:
Small cuts, scratches. Insect bites. Surgery (very rare). In some cases, the bacterial infection pathway that causes necrotizing fasciitis cannot be clearly defined. Once present, necrotizing fasciitis progresses rapidly and destroys connective tissue, fatty tissue, and muscle tissue.

Vi khuẩn ăn thịt người xâm nhập vào cơ thể con người qua vết cắt nhỏ, vết trầy xước
3. Symptoms of infection with flesh-eating bacteria
Symptoms of flesh-eating bacteria usually appear within 24 hours of infection, and often do not appear alone but appear in combination. Signs that may appear are:
Increased pain in the surrounding area of the wound, cuts, abrasions, etc. The site of the wound is much more painful than the wound can be. really caused. The area around the wound is swollen, hot, and red. Flu-like symptoms such as diarrhea, nausea, fever, dizziness, and malaise. Feeling very thirsty because the body is dehydrated. Progressive symptoms appear around the site of infection within 3 to 4 days of infection and include:
Swelling, possibly purple rash. Large areas of skin turn purple, followed by blisters filled with dark discharge with an unpleasant odor. Skin discolouration, peeling, and shedding of the skin when tissue gangrene occurs. Serious symptoms that usually occur within 4 to 5 days of infection include:
Severe drop in blood pressure. Toxic shock. Drowsiness, coma.

Ở giai đoạn tiến triển, các vùng da lớn chuyển sang màu tím
4. Diagnosis of infection with flesh-eating bacteria
Early diagnosis of flesh-eating bacteria or necrotizing fasciitis is important because the disease progresses very quickly. However, early diagnosis is not always possible because the signs and symptoms of necrotizing fasciitis are similar to those of the flu or of a non-serious skin infection.
The diagnosis of necrotizing fasciitis is usually based on progressive symptoms, such as the appearance of air bubbles under the skin. Tests of fluid and tissue samples will be performed to identify the type of bacteria the patient has been infected with.
Family members and close contacts of patients with necrotizing fasciitis should be evaluated and diagnosed if symptoms of infection are present.
5. Treatment when infected with flesh-eating bacteria
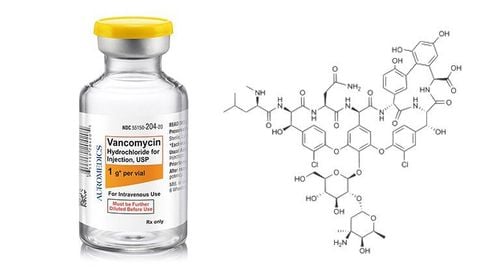
Treatment will begin before the cause of necrotizing fasciitis is identified, and the course of treatment requires a combination of different approaches. The duration of treatment depends on the specific disease condition. Treatments include:
Use of intravenous antibiotics. Surgery to remove damaged or necrotic tissue to prevent the infection from spreading. Use antihypertensive drugs. Surgery to amputate a damaged limb in some cases. Hyperbaric oxygen therapy (HBOT) to treat wounds. Cardiovascular monitoring, oxygen support. Blood transfusion. Infusion of antibodies to help fight infection.
If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: webmd.com