This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Computed tomography of the colon, also known as virtual colonoscopy (VC), was introduced in 1994 by Vining et al. They were the first to describe this modified computed tomography (CT Scan) test of the large intestine as a diagnostic test for colorectal carcinoma and polyps. Since then, virtual colonoscopy has become a test of essential importance in the imaging of polyps and occult colorectal cancer in patients unadapted to optical colonoscopy.
1. Risk of radiation exposure
The main disadvantage of virtual colonoscopy is ionizing radiation, especially because virtual colonoscopy has been considered as a screening tool for colorectal cancer. Radiation dose significantly determines CT Scan image quality, diagnostic accuracy, and clinical utility. The dose of virtual colonoscopy is lower than that of conventional CT Scan, about half the dose, due to the high natural contrast between the soft tissue of the colon wall, vaginal discharge, and fecal residue and tagged fluid. For insight, it makes sense to compare the dosages of different diagnostic procedures with the dose of chest X-rays or the number of years of exposure to natural background radiation, which ranges from 1 to 2. 3 mSv/year, depending on geographical area. Thus, mammography has a dose of 0.13 mSv, corresponding to 6 chest x-rays or 14 days of background radiation. An average abdominal CT scan has 5-25 mSv, which corresponds to 250-1250 chest X-rays or 2-11.5 years of background radiation, depending on the number of stages required to confirm the suspected diagnosis.2. CT Scan technology to find ways to reduce radiation dose for CT Scan tests
Over the last few decades, physicists, radiologists, and technicians have studied CT Scan technology to find ways to reduce radiation doses for specific "diagnostic related" CT Scan tests. . Currently, the authors have well-established “diagnostic related” procedures such as “low-dose” kidney stone-specific regimens, “low-dose” lung cancer screening protocols, and more. Dose reduction can be achieved in two ways.
First, it is important to target image quality appropriately for a particular diagnostic test, not requiring lower noise or higher spatial resolution than is necessary. For example, in high-contrast environments, as in the detection of colon polyps from the background of air and tagged stools, it allows high noise levels and relatively low radiation doses without reduced diagnostic confidence. Detection and characterization of low-contrast lesions in CT scans of hepatobiliary and encephalopathy requires relatively low noise levels and higher radiation doses. Unanimous consensus on image quality requirements exists in guidelines and standards, but exact quantification requirements exist only in some exams.
3. There are many ways to adjust the scan parameters to reduce the dose.
One way to reduce the dose is to change the exposure specifications of the scan: Tube current or voltage depending on tissue density and contrast, scan area, shape and body size of the patient. patient. Modern CT Scan equipment can automatically adjust the X-ray tube current after obtaining the initial plot of the scanned area, known as automatic tube current modulation (ATCM). The ATCM adjusts the X-ray tube currents (mAs) according to the size and attenuation of the body part examined. The use of ATCM for virtual colonoscopy has been recommended. Each change in scanning parameters affects the quality of the image, in particular the spatial resolution and/or contrast, which is important for the detection of specific pathologies. Spatial resolution is concerned with clear boundaries of tissues, organs, or structures, while contrast resolution is concerned with contrast differences of different tissues (eg, normal normal or pathologically variable). Low dose protocols have higher image noise due to altered (lower) electrical conditions. Spatial resolution or contrast is sacrificed and the radiologist must derive the same information from the detailed images.
4. It is important to balance the dose by adjusting the electrical conditions and maintaining the image quality.
Image quality should be good enough to distinguish pathological lesions from normal structures. Therefore, it is important to find the delicate balance between the lowest dose and acceptable image quality, enabling the radiologist to distinguish pathological structures. This is also known as the Achieving as Low as Possible principle, which is well established in the field of radiation protection. In addition to changing exposure parameters, software options have been developed to reduce image noise by keeping tube currents as low as possible. These software reconstruction techniques are Sinogram Confirmed Iterative Reconstruction (SAFIRE) and a conventional filtered back projection. These techniques allow even lower radiation doses to be used than the conventional low-dose (LD) protocol named ultra-low dose (ULD) with maintained image quality.
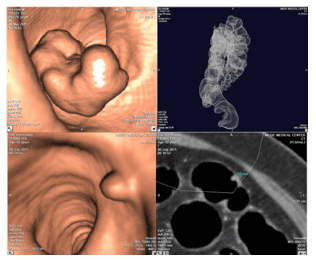
In 2018, a study evaluating the diagnostic value of the ULD protocol in the detection of polyps found that the ULD protocol reduced the effective dose by up to 63.2% compared with the LD protocol (0.98 mSv). for ULD and 2.69 mSv for LD). The image noise measurements were slightly lower with ULD (28.6) than with LD (29.8) (P = 0.09). Image quality does not differ between 2D and 3D with ULD and LD. A special 3D software option must be used to navigate the large intestine and when interpreting virtual colonoscopy to help detect intraluminal lesions. In contrast, the 2D option is the routine CT Scan technique. The polyp detection was also comparable, with no significant differences in polyp detection rates and measurements for the LD and ULD protocols. Therefore, if an iterative reconstruction method (the software option in most modern CT Scan scanners) is included in the scan, the virtual colonoscopy-ULD image quality is not compromised. significantly reduced compared with LD-virtual colonoscopy.
Advantages of specific computer software for virtual colonoscopy interpretation, allows dynamic viewing of two-dimensional axis images, multi-plane format and three-dimensional rendering, requires interactive training of the physician X-ray. Radiologists can use 2D axis imaging or 3D rendering for the primary interpretation of virtual colonoscopy, with an alternative approach dedicated to specific questions addressing a single lesion. potential. 3D reading is an additional software option that enhances polyp detection and reduces interpretation time without increasing patient dosage
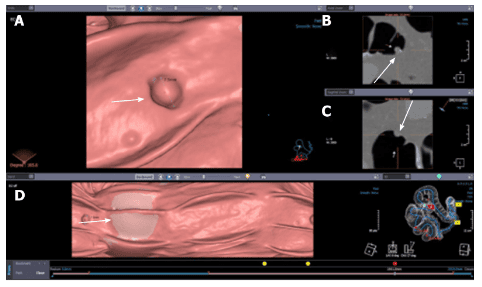
Proficient use of radiographic techniques acquired through comprehensive training correlates with polyp detection sensitivity.
Primary 2D interpretation is shown from magnified colonic axis images obtained in supine and prone positions. Compared with the main 3D interpretation, it shortens the time to evaluate lesion density and homogeneity. Stemless polyps are round or ovoid in appearance and have a soft tissue density. They remain fixed in position on the colonic wall in both supine and prone images. Stool can be distinguished from polyps because it is usually of mixed density and changes position as the patient changes position. Stem polyps may change position as the patient transitions from the supine position to the prone position, but the pedicle is usually easily identified on 2D and 3D images. Multiplane format and 3D images are useful for morphological assessment of lesions and confirmation of polyps.
In addition to widely used radiation dose reduction techniques such as automatic tube dose modulation (which automatically adjusts after the initial plot), tube current reduction, and the application of repeated reconstruction (IR), the reduction of tube voltage can be helpful. This option is rarely used for conventional CT Scans because it reduces the penetration of X-rays through the scanned area. However, during virtual colonoscopy, the bowel is highly contrasted due to the presence of gas in the vagina; Therefore, high voltage is not required. If there is an option for IR, we can reduce the voltage and enable IR.
5. The iterative reconstruction software option corrects the image noise arising from the lower voltage.
Data show that low tube voltage with IR leads to a 27% reduction in radiation while maintaining image quality and detectability (100kVp vs 80kVp). Also, new IR like SAFIRE can reduce the voltage even more. Recent studies show that both hybrid and repeat pattern reconstruction are suitable for submilliSievert superdose virtual colonoscopy without sacrificing the diagnostic efficacy of the study. Certain active factors often lead to higher doses. Repeated CT Scans, such as polyphasic tests, increase the radiation dose. For example, suppose that a diagnostic virtual colonoscopy is being performed in a patient with suspected colorectal carcinoma. In that case, intravenous contrast may be needed and CT Scan acquisition parameters will often require higher mA. If the patient is undergoing virtual colonoscopy as a screening test, intravenous contrast is not routinely used.
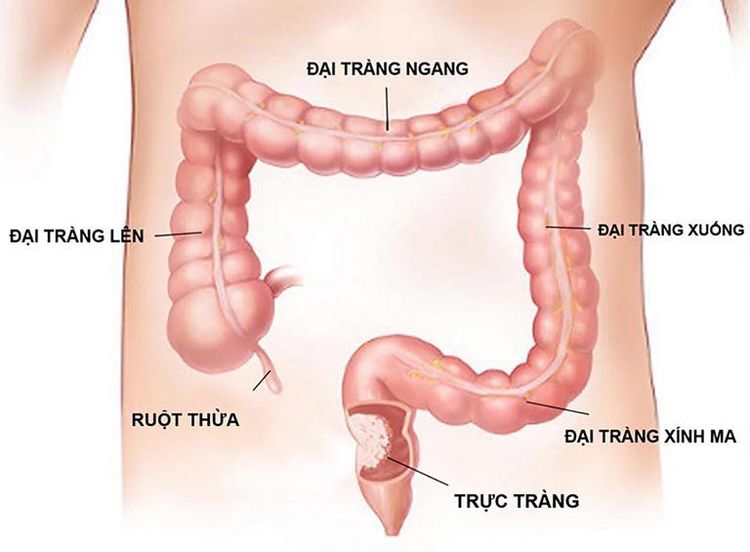
6. The height and/or length of the patient also affects the radiation dose.
Longer scan length results in radiation exposure to a larger anatomical area and thus higher radiation dose. For some reason, for detailed analysis, radiologists may require thinner images that provide better image resolution and improve visibility of small objects. However, the beam intensity needs to be increased to reduce noise in these thinner images, while increasing the radiation dose. Because the entire abdomen can be seen during a virtual colonoscopy examination, many abnormalities outside the colon can be detected. Several US screening studies have collected data on clinically significant extrasystoles that warrant further imaging.
The proportion of patients receiving a follow-up CT Scan to investigate these findings ranges from 5-10%. The most common tracking scans are; CT Scan of the abdomen and CT Scan of the abdomen/pelvis and chest. The dose from a CT scan of the abdomen/pelvis performed with and without contrast is about 20 mSv, which would result in a radiation risk twice as high as the risk from a virtual colonoscopy. However, given that only a small percentage (eg, 10%) of the screened population will receive additional scans, it is unlikely that they will increase the average risk for the entire screened population by more than 20%.
The American College of Radiology (ACR) standard virtual colonoscopy protocol specifies that the patient be scanned in both supine and prone positions to allow assessment of the entire colon with displacement dependence of vaginal discharge and the additional distension of independency. segments of the large intestine. In rare cases, the same segments of colon will collapse to the standard position, requiring a third series to complete the diagnostic evaluation.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.