This is an automatically translated article.
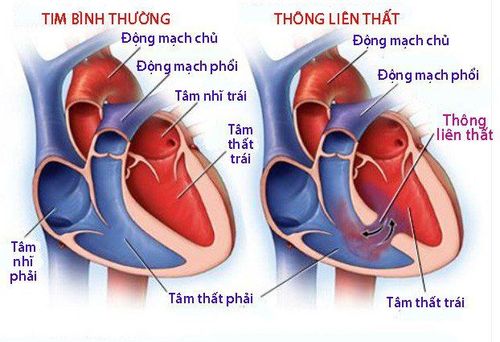
Pulmonary and valve atrophy with ventricular septal defect is a rare congenital malformation with a poor prognosis. This is a serious abnormality affecting the development of the pulmonary artery stem and the membranous portion of the interventricular septum. To avoid high mortality, children need to be diagnosed and treated promptly.1. What is ventricular septal defect, valve atrophy, and pulmonary artery?
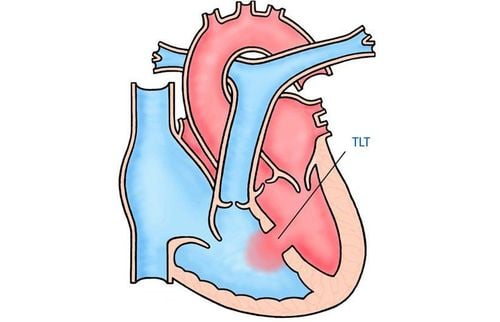
Pulmonary hypoplasia (including valve atrophy and pulmonary artery atrophy) with ventricular septal defect is one of the cyanotic congenital heart diseases. This pathology occurs due to underdevelopment of the right ventricular outflow tract along with the pulmonary valve and the main artery. This malformation is also associated with aortic compression and has a large ventricular septal defect.The severity of isthmus and pulmonary artery atrophy with ventricular septal defect varies in presentation and severity in most cases depending on the degree of pulmonary stenosis.
2. Causes of ventricular septal defect, valve atrophy and pulmonary artery disease
The cause of the disease is still unknown. However, several risk factors have been shown to be associated with this incidence, including:History of congenital heart disease in both parents. Maternal history of teratogenic drug use Smoking during or prior to pregnancy Poorly controlled diabetes Pregnancy in the elderly mother However, these risk factors are not specific for valve atrophy and Pulmonary artery atrophy is associated with ventricular septal defect as also commonly found in association with other congenital heart defects.
The prognosis of pulmonary hypoplasia with ventricular septal defect is particularly poor if left untreated. Approximately 50% of pediatric patients die within the first two years of life. With appropriate treatment and monitoring, 65% of patients alive beyond 1 year can live beyond 10 years of age.

Nguyên nhân gây bệnh thông liên thất có thể do tiền sử bệnh tim bẩm sinh ở cả bố hoặc mẹ
3. Manifestations of ventricular septal defect, valve atrophy and pulmonary artery like?
Ventricular septal defect, valve atrophy and pulmonary artery atrophy are clearly demonstrated by fetal echocardiography at 18 to 22 weeks gestation. Many cases may go unrecognized if pregnant women do not have access to appropriate maternal health care resources during pregnancy. In these situations, the diagnosis is only known after birth.The clinical presentation of ventricular septal defect, valve atrophy, and pulmonary artery atrophy is highly variable depending on the degree of pulmonary stenosis. Some common symptoms include:
Central cyanosis may manifest as a bluish discoloration of the face, especially around the mouth and lips. In severe cases, cyanosis may be seen in the peripheral extremities as well. Increased respiratory rate or dyspnea due to hypoxic blood, which may not be evident at rest and manifests only with exertion, i.e. crying or breastfeeding. Weak cry, loss of timbre and poor suckling. Difficulty suckling. Cardiovascular examination may reveal central cyanosis, a left sternal systolic murmur that may radiate to the back or axillary region. In addition, children seem to be underweight for their age and sluggish and less flexible. Peripheral edema, tremors and more severe cyanosis may be signs of congestive heart failure.
4. Tests to be done for ventricular septal defect, valve atrophy and pulmonary artery
The following tests are part of the comprehensive evaluation of infants with ventricular septal defect, valve atrophy, and pulmonary artery atrophy:Measurement of capillary oxygen to assess oxygen saturation (especially dark skin in neonates may appear cyanotic on physical examination). Arterial blood gas. Basal hemoglobin and blood cell indices. Genetic testing especially if other birth defects are present. Chest X-ray (no shadow of pulmonary artery, boot or enlarged heart, signs of poor pulmonary vasculature, etc.). Echocardiography (pulmonary regurgitation, aortic compression, atrial septal defect, pulmonary hypertension, reduced ejection fraction if heart failure is present) Magnetic resonance imaging or computed tomography (very important to confirm determine vascular anatomy prior to surgery to plan correction, which can be difficult to visualize on echocardiography). Classification of cardiac malformations and angiography (anatomical features, size and distribution of blood vessels, pressure in the right ventricle, pressure gradient across the pulmonary valve).

Tình trạng thông liên thất, teo van và động mạch phổi được phát hiện qua siêu âm thai
5. How to treat ventricular septal defect, valve atrophy and pulmonary artery?
5.1 Medicine Oxygen saturation is very important and should be monitored continuously.Similarly, fluid balance and acidosis, if present, should also be addressed urgently. Because infants with ventricular septal defect, valvular atrophy and pulmonary atrophy in general, or congenital heart disease are often unable to suckle well, nutritional rehabilitation may also be necessary.
In severe valvular cases, the pulmonary artery is incompletely formed, and the pulmonary circulation is completely dependent on the ductus arteriosus, a prostaglandin E2 infusion that maintains the aortic valve open until surgery can be performed adjust.
In addition, symptomatic treatment with diuretics or digoxin is also indicated if the patient is at risk for progression to congestive heart failure.
5.2 Surgery The surgical management mainly depends on the size of the pulmonary artery and the presence or absence of ductus arteriosus to guide the surgical plan. Although the surgical revision approach has not reached a comprehensive consensus due to the wide variation in anatomy, staged palliative surgery is preferred by most surgeons over corrective intervention. early overall.
Accordingly, the correcting steps are in phased palliative therapy:
Blood flow is first established in the pulmonary arteries by direct connection to the aorta through a Blalock-Taussig shunt. be modified. The right ventricle is also temporarily connected to the aorta if overload is insufficient. As the pulmonary arteries grow in size as the blood supply from the aorta is maintained, the pulmonary circulation is then connected to the pulmonary artery. The right ventricle is connected back to the pulmonary artery. By the time the child is six months old, if the respective lobes have received adequate supplies through temporary pulmonary artery modification, the pulmonary artery has been relatively developed. The ventricular septal defect is repaired alone between the ages of 1 and 3 years. The main benefit of this point is that the child has reached a sufficient level of fitness for intervention. 5.3 Early Comprehensive Repair In contrast to staged repair, another approach is complete repair in one surgery. This procedure is only suitable for children with severe degrees of congenital heart disease.
Accordingly, because the infant's physical condition is still weak, pediatric patients should be carefully selected and the possible risk versus benefit comparison should be carefully analyzed before choosing this option. .
5.4 Heart Transplant In patients whose pulmonary circulatory system is completely dysfunctional or who have failed surgical corrections, a heart transplant may be a viable option.

Điều trị tình trạng thông liên thất, teo van và động mạch phổi bằng cấy ghép tim
6. Complications of ventricular septal defect, valve atrophy and pulmonary artery
In addition to surgical and anesthetic complications in selected patients for intervention, some complications of ventricular septal defect, valve atrophy, and pulmonary artery atrophy that can be acquired are:Congestive heart failure Reactive erythrocytosis response to chronic hypoxia Infective endocarditis due to abnormal blood flow Sepsis due to infective endocarditis or underdeveloped immune system Developmental delay Arrhythmia Sudden death Summary, Ventricular septal defect, valvular atrophy, and pulmonary artery atrophy is a rare congenital heart disease and has many clinical signs and symptoms that overlap with other congenital malformations. Therefore, infants need to be evaluated comprehensively to make a final diagnosis. At the same time, the treatment process also needs to coordinate with many different specialties such as pediatric cardiology, pediatric surgery, genetics doctor,...
However, the most important thing is the prenatal check-up during pregnancy. during pregnancy, in order to detect early and have appropriate treatment from the beginning. Therefore, to detect congenital heart defects as early as possible and protect the health of mother and baby comprehensively. Vinmec also offers a package of maternity services to promptly recognize abnormalities during pregnancy, help monitor the health of mother and baby right from the beginning of pregnancy, detect and intervene early on problems. health issue.
Along with comprehensive health care services, the Cardiovascular Center, Vinmec International General Hospital is also one of the leading spearhead centers, with a full team of experts including: Professor, Doctor, Specialist 2, Master have experience, great reputation in the field of medical treatment, surgery, interventional cardiac catheterization and application of advanced techniques in diagnosis and treatment. treatment of cardiovascular diseases.
In particular, the Center has modern equipment, on par with the most prestigious hospitals in the world. This is also the first private hospital and the second hospital in Vietnam to successfully implement the HVAD ventricular-assisted artificial heart transplant technique. Performed 18 transcatheter aortic valve replacement - One of the most complex cardiovascular intervention techniques in the world today within more than 1 year; performed the first MitraClip case and hundreds of aortic and coronary interventions, including complicated and difficult-to-access cases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.