This is an automatically translated article.
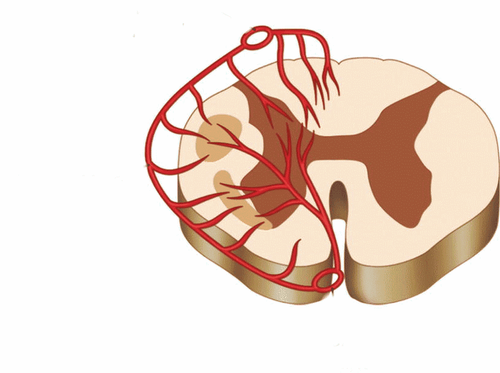
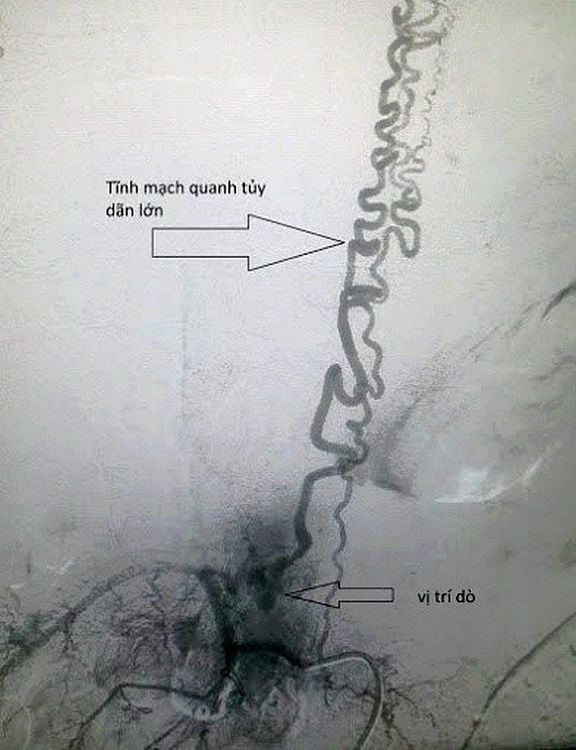
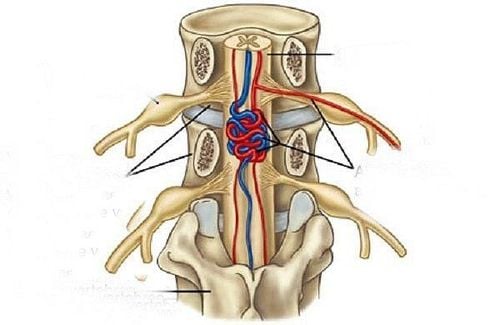
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International Hospital.Spinal arteriovenous malformations (AVMs) are the second most common spinal vascular anomaly after dural arteriovenous fistulas, accounting for 15% of all spinal vascular malformations. Typically, the anterior and posterior spinal arteries supply arterial blood to abnormal intramedullary or perimedullary foci or cavities, and then drain blood into a spinal vein.
Part III: Arteriovenous fistula of the spinal cord
1. Dynamic malformation - Spinal vein
Spinal arteriovenous malformations are the most common cause of non-traumatic spinal hematomas and occur in about half of patients. The annual bleeding rate is 4%, although it increases to 10% if there has been previous bleeding. Vigorous catheterization induces the formation of aneurysms within the malformation in 30% to 40% of cases, and their presence increases the bleeding rate.In non-bleeding venous-dynamic malformations, symptoms are due to mass effect, vascular stealing, venous thrombosis, or venous congestion, although the latter is less common than in dural arteriovenous fistula.
Patients with spinal venous malformations usually present in the 30s, although manifestations in adolescence and later are also present. There is no gender preference, but they can be seen in inherited syndromes such as hereditary hemorrhagic astrocytoma and Cobb's syndrome (a rare genetic disease characterized by skin lesions and myeloma or anomalies). spinal venous form). The majority of spinal venous malformations (about half) are found in the thoracic medulla.
Patients with marrow hematoma present with severe back pain and symptoms of acute myelopathy. More gradual myelopathy symptoms may be seen in non-bleeding venous-dynamic malformations.
Customers can refer to:
Notes when magnetic resonance imaging (MRI) brain and spinal cord MRI is usually a diagnostic test, showing mixed signals on intramedullary or extramedullary T1 and T2 in the context of bleeding and increased intramedullary T2 signalling, with spinal edema in patients with symptomatic but non-bleeding lesions. Increased contrast enhancement is not constant, and voids of flow due to dilated vessels are common. Routine angiography is key to determining the structure of the vascular lesion and planning treatment.
Embolization and surgery are options for the treatment of spinal arteriovenous malformations ; however, their success rates are lower than spinal arteriovenous fistulas (33% and 78% for embolization and surgery, respectively). This is because the arterial blood supply to the spinal venous malformation often also perfuses the spinal cord, increasing the risk of spinal ischemia during treatment.
2. Other spinal vascular diseases
2.1 Cavernous malformations Cavernous malformations of the spinal cord (also called cavernous angiomas or cavernous hemangiomas) include dilated and thin-walled sinusoidal veins and no identifiable feeding artery or vein conduction circuit. About half of patients have slowly progressive symptoms due to increased size of cavernous malformations due to microbleeds, while the other half have acute or progressive symptoms due to internal or pulmonary bleeding. around the cavernous malformation.
Spinal cavernous malformations are common in the fourth decade and are mildly predominate in males. A family history of cavernous malformation was seen in 12% of patients, and 17% of patients had an associated intracranial cavernous malformation. About 90% of cavernous malformations are in the neck or chest. The annual bleeding rate is 2.1% to 3.9%, which is higher than with brain injury.
Sensory motor symptoms below the level of injury are the most common symptoms. Pain is present in up to a third of patients and may precede the sensory symptoms by several hours. About a quarter of patients have bowel or bladder dysfunction. Cavernous malformations not visible on angiography; MRI is the diagnostic method of choice.
Well-defined lesions with heterogeneous signals within the lesion on T1 and T2 pulses, giving cavernous malformations a "popcornlike" appearance due to blood products in in different phases, most visible on the echo gradient pulse.
In addition, there is a hypoechoic border surrounding the lesion, indicative of hemosiderin. There may be calcification, although less common than with brain lesions. Increases in contrast enhancement, if any, are usually minimal. The differential diagnosis may include intramedullary tumors (especially hemangioblastomas) and spinal venous malformations. Angiography may be considered to rule out spinal arteriovenous malformations if clinically indicated.
Carefully selected patients for surgical resection will have a higher rate of symptom improvement and clinical stability and a lower rate of severe progression, even with partial resection of the lesion. . Better outcome is achieved with surgery within 3 months of symptom onset and with a posterior semicircular approach. In contrast, conservative treatment is recommended in asymptomatic, mildly symptomatic, or elderly patients.
2.2 Epidural Hematomas Spinal cord epidural hematomas originate in the medial vertebral venous plexus and cause symptoms by pressing on the spinal cord. Risk factors include advanced age, spinal surgery/procedure, and use of anticoagulants. Epidural hematomas typically extend across 4 vertebral segments and are most common in the mid cervical and lower thoracic spinal cord regions.
Severe back, neck, or radicular pain, followed by progressive autonomic/sensory deficits that increase in proportion to spinal cord injury. Progression can be rapid, resembling a spinal infarction. CT can diagnose the disease, showing a lenticular compression mass.
However, MRI is more sensitive; epidural hematomas are non-enhanced and hyperintense to iso- signal on T1 and hyperintense on T2, although a heterogeneous signal pattern may be encountered, particularly in the case of antiretroviral therapy. bronze.
Treatment of spinal epidural hematomas is surgical removal of the hematoma. Significant improvement is possible with treatment, and, in most cases, patients can expect an improvement of at least one order of magnitude according to ASIA. In contrast, patients with mild symptoms or no symptoms can be managed conservatively. Poor prognostic factors for outcome included initial clinical severity, motor and sensory symptoms, thoracic spinal cord involvement, and prolonged hematoma.
Vascular diseases of the spinal cord can be suspected in patients with risk factors and presenting with symptoms of both acute and progressive myelopathy, often with pain. MRI is essential for the diagnosis of vascular diseases of the spinal cord.
However, routine angiography, selectively based on prior MRA, is essential to confirm the diagnosis of dural arteriovenous fistula and spinal arteriovenous malformation and provide information decisive for treatment.

Appropriate and prompt treatment, often in conjunction with a neurosurgeon or an interventional neurologist, can result in clinical improvement in nearly all cases of myelopathy vascular origin.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced. .
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to the source:
Kramer CL. Vascular Disorders of the Spinal Cord. Continuum (Minneap Minn) 2018;24(2, Spinal Cord Disorders): 407–426.