This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Previously, the treatment for resectable pancreatic ductal carcinoma was surgery, followed by adjuvant chemotherapy. In 2008, a large retrospective study showed that adjuvant treatment of neoplasia after surgery had a survival advantage over preoperative surgery with or without adjuvant therapy, suggesting the role of adjuvant therapy. adjuvant neoplasia in the treatment of reversible pancreatic ductal carcinoma.
1. Overview
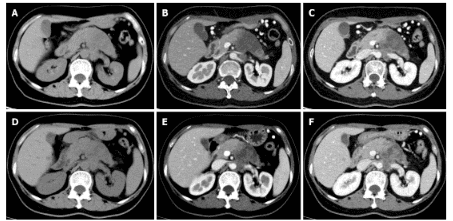
Pancreatic ductal carcinoma has become a major global public health problem. Due to the late onset of symptoms, the high invasiveness of the disease, and the lack of accurate diagnostic markers to detect micrometastasis, the prognosis of pancreatic ductal carcinoma has not been significantly improved over many decades. past century. Neoplastic adjuvant therapy (NAT) is an emerging therapy for pancreatic carcinoma. It offers the theoretical advantages of locally advanced or resectable pancreatic tumors, allowing more patients to benefit from surgery, increasing R0 resection, treating metastases micro and prolong survival (OS). With advances in imaging technology and new interest in data collection and analysis, an increasing number of studies report the accuracy of imaging to assess response to neoplastic adjuvant therapy. for pancreatic carcinoma.2. Strategies for classification and treatment of pancreatic ductal carcinoma
Various guidelines recommend using multiphase contrast-enhanced computed tomography (CT) imaging to stage pancreatic ductal carcinoma and determine resection potential.
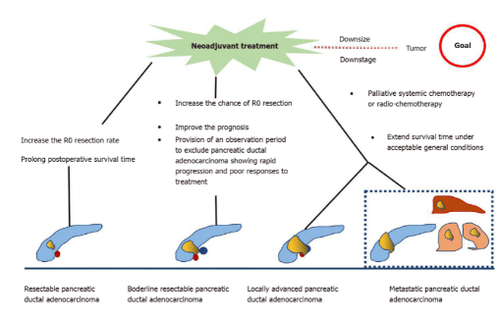
According to the National Comprehensive Cancer Network guidelines, pancreatic ductal carcinoma can be divided into 4 types. The following is a classification of pancreatic ductal carcinoma based on a preliminary assessment of tumor location and metastasis:
Reversible: The likelihood of R0 being resected is very high. Tumor does not contact adjacent arteries [superior mesenteric artery, hepatic artery, or gastric artery (CA)] and veins [superior mesenteric vein (SMV), portal vein ( PV) or their confluence (SMV/ PV)] or the degree of contact is less than 180° of the circumference of the vessel wall; Contour retouchable: The possibility of incomplete resection of R1 or R2 is high. The degree of contact between the tumor and the artery (superior mesenteric artery or CA) is less than 180°, and the tumor invades a short segment of the hepatic artery that can be surgically or reconstructed, but is not involved. CA, or tumor in contact with an adjacent vein (SMV-PV) beyond 180° of the circumference of the vessel wall; Local enhancement: The tumor cannot heal due to invasion of nearby structures; Metastasis: The tumor has metastasized. As seen from this classification, the exposure of the tumor to the blood vessel is important to determine if the tumor is resectable. At the same time, performing R0 resection (marginal negative resection - area free of cancer cells) is the key to prolonging the survival of pancreatic carcinoma patients. Surgical resection is recommended for operable pancreatic ductal carcinoma, and the 5-year survival rate for R0 resection is 18-24%. However, the 5-year survival rate of pancreatic ductal carcinoma at the border of radical and local surgery is poor, about 8-11%. In addition, nearly 50% of patients relapse shortly after tumor resection.
3. Neoplastic adjuvant treatment for resectable pancreatic carcinoma
Previously, the treatment for resectable pancreatic ductal carcinoma was surgery, followed by adjuvant chemotherapy. In 2008, a large retrospective study included surgically resectable ductal adenocarcinoma and investigated the impact of adjuvant neoplasia on the prognosis of pancreatic ductal carcinoma. surgery possible. The results show that adjuvant neoplasia after surgery has a survival advantage over prior surgery with or without adjuvant therapy, which suggests a possible role of neoplastic adjuvant treatment in The treatment of pancreatic ductal carcinoma can be resumed.
A recent meta-analysis showed that the mean OS of patients with adjuvant neoplasia was longer than with surgery (18.8 months vs 14.8 months). Although the overall resection rate with neoadjuvant therapy was lower than with prior surgery (66% vs 81.3%), the R0 rate was higher (86.8% vs 66.9%). In addition, other studies have reported that tumor resection rates after neoadjuvant therapy are between 50 and 90%, with a median survival of 23.5 months
4. Adjuvant treatment of pancreatic ductal carcinoma inoperable or borderline radical surgery
Accumulating evidence indicates that patients with pancreatic carcinoma at the surgical boundary may benefit from adjuvant neoplasia, as it increases the chance of R0 resection, improving the likelihood survival and identification of cases of pancreatic ductal carcinoma that progressed rapidly and responded poorly to treatment.
An international consensus has suggested that patients with radical surgically borderline ductal adenocarcinoma be surgically resected after adjuvant neoplasia in the absence of contraindications to resolution. surgery or metastatic disease. A multicenter trial found that neoadjuvant S-1 therapy combined with postoperative radiotherapy achieved an R0 resection rate of 63%.
Inoue et al. reported that adjuvant treatment of neoplasia with gemcitabine and nab-paclitaxel improved tumor degradation and enabled patient selection. Anger et al investigated the role of neoplastic adjuvant therapy in different types of pancreatic ductal carcinoma at different radical resection according to international consensus criteria. Their results suggest that patients with curatively borderline pancreatic ductal carcinoma have a relatively poor prognosis and should be considered for multimodal neoadjuvant therapy.
In unresectable pancreatic ductal carcinoma, palliative systemic chemotherapy is often used. In these patients, the primary goal is to prolong survival in generally acceptable conditions. The FOLFIRINOX and gemcitabine regimen in combination with other agents is the preferred regimen for patients with good performance status, while capecitabine, gemcitabine, and 5-fluorouracil monotherapy is usually given to patients with a general condition. least.
In summary, neoplastic adjuvant therapy for resectable pancreatic ductal carcinoma performed before primary surgery increases the R0 resection rate and prolongs postoperative survival. In radical and unresectable pancreatic carcinomas, adjuvant neoplasia increases the chance of R0 resection, providing strong evidence for individual patient management, ultimately. leading to longer survival time. However, there are some limitations in the current study. First, there is a lack of consensus on the best regimen for adjuvant neoplasia; Second, some studies have failed to clearly separate reparable ductal adenocarcinoma from unrepairable ductal adenocarcinoma during adjuvant neoplasia. Finally, there is no clear consensus on the duration of neoplastic adjuvant therapy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Zhang Y, Huang ZX, Song B. Role of imaging in evaluating the response after neoadjuvant treatment for pancreatic ductal adenocarcinoma. World J Gastroenterol 2021; 27(22): 3037-3049 [DOI: 10.3748/wjg.v27.i22.3037]