This is an automatically translated article.
The article was written by Master - Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalSince the recognition of adenomatous polyps as a precursor to colorectal cancer (CRC), the early identification and treatment of colonic lesions has received great attention. Colorectal polypectomy has become a means of cancer prevention with evidence of a reduction in the predicted morbidity and mortality from colorectal malignancies
1. Overview of colon cancer colonoscopy
Colonoscopy has been shown to be effective in detecting and removing precancerous and cancerous lesions early and, therefore, colorectal screening programs are being prepared or implemented. present around the world. Screening efforts are reducing the incidence of colorectal cancer and allowing colorectal cancer to be diagnosed at an earlier stage. Endoscopic mucosal resection (EMR) and submucosal dissection (ESD) provide means to treat lesions that previously required surgical intervention.
Despite organizational and technical improvements, current endoscopic surveillance does not provide 100% protection against colorectal cancer. The extent to which colonoscopy can reduce colorectal cancer rates. Suggested reasons for colorectal cancer after colonoscopy include incomplete examination, inadequate bowel preparation, incomplete polypectomy, and missed flat lesions. Colonoscopy reveals an adenoma missed rate of up to 27% and flat lesions, notoriously easy to miss, may account for nearly 40% of adenomas in the Western series.

2. Some difficulties of colon cancer colonoscopy
It is recognized that right-sided lesions are particularly difficult to identify, in part due to the difficulty in assessing the entire mucosal surface in the proximal colon. In addition, glandular changes were found in smaller proximal lesions, compared with distal lesions. Proximal serrated polyps are considered another cause of reduced effectiveness of colonoscopy examination. The term includes traditional serrated, sessile, hyperplastic polyps, previously thought to be benign but recently suggested, some with cancerous potential.Despite this, the risk of proximal colorectal cancer is related to the skill of the performing endoscopic surgeon rather than to any patient or polyp characteristics.
Every endoscopist should actively look for proximal and flat or concave lesions. For the general endoscopist, the ability to accurately find and evaluate a lesion is critical. Advanced endothelial treatments mean that more lesions are potentially removable and so the endoscope must be able to describe lesions in a standard way whether removed at home or transferred to the tertiary unit.
3. The essentials of the pretreatment phase
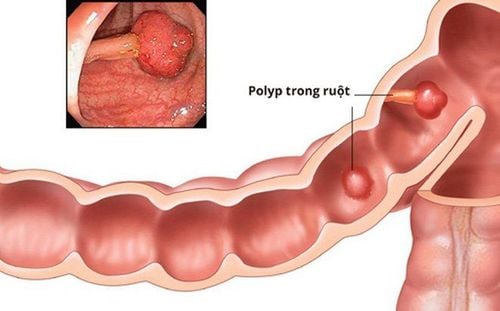
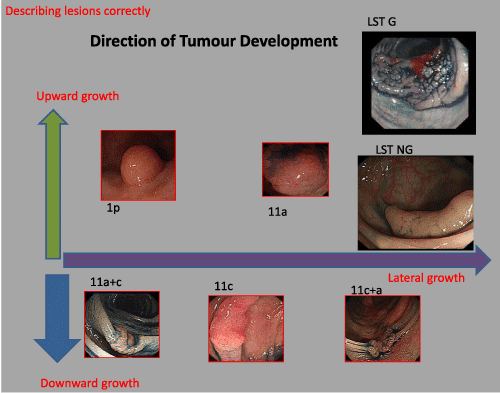
The ability to accurately classify lesions is key to early colon cancer treatment.Unlike the upper gastrointestinal tract, the colorectal mucosa has no lymphatics in the mucosa, so mucosal lesions do not pose a risk of lymphatic metastasis. If the carcinoma is located entirely within the mucosa, the risk of lymph node and vascular invasion is zero and as a rule, endoscopic resection is appropriate for such lesions. Lesions may grow upward, downward, or form adjacent. This shows potential for submucosal invasion, thus making it suitable for endoscopic intervention.
The Paris Classification provides a simple and internationally valid classification that allows an accurate, standardized method for describing the macroscopic appearance of superficial tumors from the esophagus to the colon. It allows to predict the possibility of submucosal invasion and, therefore, to decide whether a lesion can be safely removed at the time of index endoscopy, based on the EMR by the physician.
4. Optimizing colonoscopy to aid in early colon cancer detection and classification
Recognizing that colonic lesions were missed, efforts were made to optimize mucosal assessment and visualization. Fundamental improvements, such as optimizing bowel preparation and ensuring a minimum number of individuals per year for endoscopy, have contributed to the reduction in missed adenomas. Minimal drug discontinuation has been shown to increase ADR (endoscopic detection rate of adenomas) and is now accepted as the standard in all endoscopic procedures, while patient position changes. regional changes in the bowel, and the routine use of buscopan during intubation, have been suggested to improve mucosal imaging. Other groups have focused on adjuncts to endoscopy, such as endoscopes with flaps, retrograde colonoscopy, and extended views.In addition to bowel optimization and endoscopic techniques, image-enhanced endoscopy is increasingly being used. Many studies have examined its use, both to aid in detection and to aid in histological diagnosis.
Standard white light endoscopy relies on careful assessment of slight color changes (pale red or discolouration), mucosal abnormalities, and disruption or loss of underlying vessels. It is considered inaccurate in histological classification prediction.
4.1. Endoscopic staining is the first aid method for lesion assessment
Originally, staining endoscopy was described as the use of carmine indigo as a means of creating contrast between normal and abnormal mucosa. A 2010 meta-analysis of five randomized controlled trials estimated a 50% increase in polyp detection.The application of staining endoscopy has been limited because it is laborious and time consuming and does not allow switching between chromoscopic and conventional views. There are efforts to use new techniques for contrasting coloration, including the use of slow-release tablets, but newer endoscopes aim to provide a virtual means of appreciating features. similar without imitation.
4.2. High definition white light endoscope
Studies show great promise in distinguishing between adenomatous and hyperplastic polyps, and new generations of endoscopy hold the promise of making new techniques easier to apply. The Kudo system, using high-definition white light endoscopy, provides an additional means of stratifying the risk of submucosal invasion or malignancy. Kudo is a currently well-described means of describing mucosal pit models. Developed in Japan, it has proven to be an accurate means of classifying polyps prior to formal histological evaluation.In addition to assisting in the identification of polyps, it is suggested that high-definition white light endoscopy can also improve the detection of lesions, especially small, flat, right-sided adenomas. . However, there is still no evidence that this has a significant effect on patient outcomes.
4.3. Virtual image processing
Narrowband imaging uses a light filter to narrow the bandwidth of light coming from the endoscope. The resulting blue-green light spectrum highlights mucosal vessels and results in an impression of pitting pattern. Post-processing imaging techniques such as FICE (Fujinon Smart chromoendoscopy) and iSCAN use computer algorithms to further highlight mucosal features.Sano classification uses visualization of microvessels and pit-like patterns of polyps seen by narrow band imaging to distinguish between adenomatous polyps and carcinomas. The prediction of NBI in histology is highly accurate, but there is still no evidence that the initial detection rate is significantly increased.
The confident use of endoscopic lesion recognition adjuvants has allowed the American Gastrointestinal Association to recommend a “resect and remove” treatment algorithm. Accordingly, after optical assessment, lesions <5mm were either left in situ or excised and removed without histopathological analysis. This is expected to make the best use of endoscopic resources and prevent putting patients at risk for unnecessary laparoscopic surgery. However, while the imaging enhancement techniques have proven to be accurate in high volume centres. Wider adoption in non-specialist centers is less certain due to unacceptably low rates of sensitivity and specificity.
5. Approaches when considering polypectomy
There are different areas to consider when assessing the suitability of a lesion for polypectomy. Several approaches are available, ranging from conventional polypectomy for lesions less than 20mm, to EMR (endoscopic mucosal resection) or ESD (endoscopic submucosal dissection) for major lesions or surgery. better, whether laparoscopic-assisted resection (LAC) or open surgery, if there is deep invasion. A suitable, readily available support frame is important prior to any endoscopy. This is even more important if there is a chance that larger polyps, with a higher chance of complications, can be removed. Familiar kits and appropriately trained nursing staff should be available. The endoscopist must be appropriately trained and mentored. Support staff including surgeons, pathologists and operating managers are essential.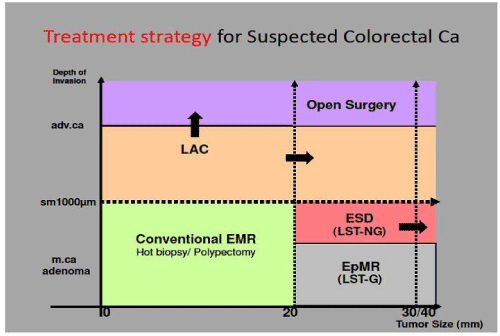
Finally, before removal, all hazards should be considered. Right-sided lesions, especially those of the caecum proximal to the appendix and those proximal to or involving the diverticulum, should be encouraged with caution due to the increased risk of perforation. There may be significant scarring from a previous ablation attempt, which can make the procedure more technically difficult.
6. Future direction
Colonoscopy is effective in reducing the incidence of colorectal cancer, however, it does not simply “go around” to the cecum. Endoscopic technology has advanced tremendously in the past years and will continue to do so in the future. We can now assess and classify lesions with increasing confidence, to the extent that excision and removal methods are being advocated by national authorities, eliminating the need for assessment. Histological evaluation of selected lesions.The definition of an endoscopically treatable lesion is changing. Precise assessment of invasiveness, together with new equipment and techniques, allows the endoscopic surgeon to remove the previously mentioned lesions for surgery. The importance of good bowel preparation, technique and proper withdrawal time is now recognized as crucial in optimizing polyp detection rates. Complex lesions are best managed in high volume specialist centres, it is more important that every endoscopic surgeon uses the Paris Classification as a means of assessing and describing any lesions reported found, whether removed or moved.
Although additional techniques such as narrowband imaging or high-definition white light microscopy may not be widely available, simple, universally applied approaches have been shown to be improved lesion detection rate. The utility of advanced technology has been demonstrated in specialist centers in discriminating between lesions. As its availability expands and its application expands, it is likely that its use will become more widespread, and the requirement to incorporate endoscopic training programs seems inevitable.
In summary, an appreciation of the techniques available, together with the proposed management strategy, will allow for useful introductory information. This will lead to optimal management of early colonic neoplasms.
Colorectal cancer is completely curable if detected early, so screening for early detection of colorectal cancer is very important. When there are risk factors or suspicious symptoms, you should go to hospitals and specialized medical centers for screening to help detect colorectal cancer early.
Vinmec International General Hospital is a large hospital chain, the first general hospital in Vietnam to meet global medical standards. Currently, Vinmec is a leading medical facility in the field of colorectal cancer screening and detection.
Vinmec International General Hospital is one of the hospitals that ensures modern equipment, a team of doctors, good and experienced staff with leading professors and doctors at home and abroad. Preventive, advanced tests allow the implementation of the most advanced colorectal cancer screening techniques.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: K McWhirter, R George and YAng. State of Art Update: Detection and Classification of Early Colonic Neoplasia