This is an automatically translated article.
The article was professionally consulted with Master, Doctor Truong Thanh Tam - Pediatrician at the Department of Pediatrics - Neonatology - Vinmec Danang International General Hospital.Mortality from septic shock in children is among the leading causes of death in developing countries. Early recognition and timely management of symptoms with aggressive measures of fluid resuscitation in the first hour, use of vasopressors and appropriate inotropic inotropy help reduce mortality from septic shock.
1. What is septic shock?
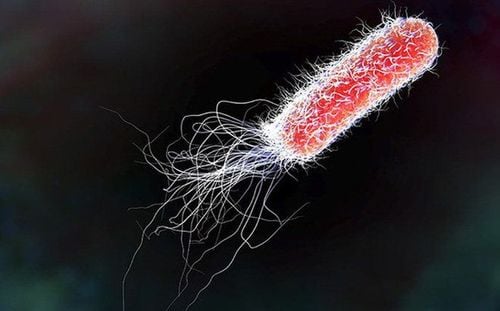
Shock is a state of acute circulatory failure that causes tissue perfusion less than required, resulting in a decrease in the supply of oxygen and glucose as well as a decrease in the removal of cellular metabolites such as lactic acid, CO2. If not treated in time, it will progress to cell damage, multi-organ damage leading to death.Septic shock is a state of acute circulatory failure that causes reduced organ perfusion, promotes systemic inflammatory reactions and prolonged metabolic disturbances, leading to multi-organ failure and death
Viruses and fungi are also causes septic shock, but more commonly bacteria. Most bacteria can cause bacteremia, but bacteremia does not necessarily progress to septic shock. Blood cultures are positive in only 30-50% of patients with severe infections.
2. Diagnosis of septic shock in children
2.1. Ask about the onset of symptoms: Help identify the primary source of infection and identify the causative agent. Painful urination, urinary incontinence, frequent urination (UTI). Diarrhea, bloody diarrhea (digestive infection). Skin boils, abscesses (staphylococci). Fever, cough (pneumonia). Vaccination status: Haemophilus, meningococcal. Risk factors: Neonatal malnutrition Immunodeficiency Immunodeficiency Agranulocytosis Corticosteroid therapy Hospitalization Invasive procedures, central venous catheterization Insplenic malignancy Malignant disease Bone marrow transplantation Organ transplantation 2.2. Clinical examination Signs of shock: lethargy, lethargy, restlessness, tachycardia, cool extremities, skin rash, blood pressure stuck, drop, CRT > 2 seconds, oliguria. Increased or decreased temperature, rapid breathing. Infectious foci: skin, incision, lung, gastrointestinal tract, urinary tract, musculoskeletal. Erythema, ecchymosis, erythema. 2.3. Laboratory tests Tests to confirm or suggest sepsis Complete blood count, hematology (blood count). CRP or PCT. Serology for suspected typhoid, leptospira PCR detects bacterial genetic molecules Total urinalysis Test white blood cell count in sterile body fluids (peritoneal, pleural, fluid) cerebrospinal fluid,...) Blood culture Specimen culture of suspected foci of infection: pus, urine, stool, cerebrospinal fluid, bone marrow X-ray of lungs Abdominal ultrasound for infection, deep abscess Test Assess sepsis severity Hepatic function Renal function Arterial blood gas Total coagulation: aPTT, PT, blood fibrinogen Lactate Electrolytes, anion gap, blood glucose/dextrostix (rapid blood sugar).3. Treatment regimen for septic shock in children
3.1. Principles of treatment Treatment of shock. Antibiotic treatment. Treatment of complications. Drain pus, if present. 3.2. Shock resuscitation for children over 1 month of age: initial treatment of septic shock Treatment of shock3.2.1. First 0-5 minutes Open airway, provide respiratory support (oxygen, intubation, early mechanical ventilation if breathing is ineffective, unstable shock, worsening consciousness). The sedation used during intubation is midazolam or fentanyl or ketamine. Establish an intravenous line or a bone marrow injection. Antibiotic injection Blood test.

Lactate Ringer or Normal saline 20ml/kg/5-15 minutes can repeat electrolyte solution to 60ml/kg and use of adrenaline.
Note: children with anemia, severe malnutrition, Thalassemia, malaria, nephrotic syndrome, pneumonia, congenital heart disease,... anti-shock fluid rate: 15-20ml/kg/hour
Total volume of fluid average 40-60ml/kg in the first hour.
In the absence of clinical improvement and normal cardiac function, excluding myocarditis, total fluid volume may be as high as 200 mL/kg in the first few hours.
Monitor every 5 minutes heart rate, rales, jugular veins, liver size, lip color, use of accessory respiratory muscles to avoid the risk of fluid overload.
Treat hypoglycemia, hypocalcemia if any.
b) Evaluation of shock response to fluid therapy
Good response: improvement in M, BP, CRT < 2", urine output: maintenance fluids
Failure to respond to total electrolytes 60ml/kg: use Use 5% albumin solution, Gelatin macromolecule solution or HES (dose ≤ 20ml/kg) and low dose adrenaline 0.05 - 0.3μg/kg/min, after 5-10 minutes, re-evaluate:
Shock Cold: continue infusion of adrenaline 0.3-1μg/kg/min. If adrenaline is not available, use dopamine at a dose of 5-9 μg/kg/min. Warm shock: low dose noradrenaline infusion 0.05-0.3μg/kg. If noradrenaline is not available, use dopamine at doses ≥ 10 μg/kg/min. Measure and monitor: Central venous pressure, invasive arterial blood pressure, catheterization to monitor urine output.
Measure cardiac output by means of PiCCO or PRAM or ultrasound, systemic vascular resistance.
Maintenance fluids CVP 8-12cmH2O (6-9mmHg).
If mechanical ventilation: maintain CVP 12-15cmH2O (9-12 mmHg), mean blood pressure (systolic blood pressure) – CVP
55 + 1.5 x age (mmHg), central venous oxygen saturation ( ScvO2) ≥ 70%, Lactate < 2mmol/L, Lactate clearance ≥ 10%/1-2 hours
If still not responding:
Normal systolic blood pressure: ScvO2 < 70%, infuse Dobutamine 5-15μg/kg/min . If dobutamine is not available, Milrinone 0.25-0.75 μg/kg/min can be used. Systolic blood pressure drop: ScvO2 <70%: increase adrenaline dose (0.4-1.5μg/kg/min), if not responding, combine with noradrenaline to achieve normal diastolic blood pressure. If cardiac output is low, add dobutamine. ScvO2 ≥ 70%: Infuse or increase the dose of noradrenalin 0.1-1 μg/kg/min. Hydrocortisone
c) If shock persists
Identify and treat pneumothorax, pericardial effusion, hypothyroidism, blood loss, increased intra-abdominal pressure, immunocompromised/disordered , control infection foci, necrotic tissue.
d) If all of the above fail:
Consider performing ECMO (extracorporeal oxygen exchange membrane) if possible.
e) The dose of vasopressor used
Adrenaline 0.05-2 g/kg/min, can be up to 5g/kg/min Dobutamine 5-20g/kg/min Dopamine 5-15g/kg/min Noradrenaline 0, 05-1g/kg/min, up to 5g/kg/min Milrinone 0.3-0.75g/kg/min, up to 1g/kg/min f) Three measures to improve ScvO2 < 70%
Maintenance fluids CVP 12-16 cmH2O Blood transfusions raise Hct > 30% or Hb > 10g%. Newborns with blood transfusion raise Hb > 12 g % Increased contractility: dobutamine or milrinone or levosimendan. 3.3. Care in the pediatric emergency department in the first 1-3 hours Early respiratory control: respiratory support, intubation if the child shows signs of increased work of breathing, worsening consciousness. Set up 2 intravenous lines under the support of ultrasound or peripheral angiography, or injection of bone marrow Anti-shock fluid: the first choice of fluid is electrolytes Infusion of vasopressors Correction of hypoglycemia, hypocalcaemia Antibiotics after blood culture Measure and monitor CVP (under ultrasound guidance, invasive arterial blood pressure (DBP), catheterization Tests: Identify infection: hematology, CRP/PCT, blood culture, specimen outside blood Assessment of severity: arterial blood gas, liver and kidney function, ionogram, blood glucose, chest X-ray, abdomen, echocardiogram to assess cardiac function, total urinalysis Monitor for shock: Lactate/1 -2 hours, blood gases/hour, ScvO2/hour for the first 3 hours 3.4 Care team in the pediatric intensive care unit for the next 3-6 hours Continue to provide respiratory support Continue to give shock resuscitation according to desired goals Continue vasopressor according to the protocol Measure CVP, BP, and catheterize if not performed Lactate, PA, ScvO2/hour x 3 hours next Assess infection status, severity if lacking
4. Antibiotics

5. Treatment of complications
Correction of electrolyte disturbances: hyponatremia, hypokalemia, hypocalcaemia Control hypoglycemia by infusion of electrolyte-containing phase fluids, hypertonic sugar (10-12.5%) by peripheral intravenous infusion, higher than in the central vein, control hyperglycemia with a goal of keeping blood glucose <180mg% using low-dose insulin 0.05IU/kg/hour and avoiding hypoglycemia. Monitor blood glucose every 1-2 hours until stable, then every 4-6 hours. Coagulation disorders: Infusion of frozen plasma, frozen precipitate and platelets in the presence of clinical bleeding and laboratory coagulopathy. There is no indication for transfusion of blood products in the absence of clinical bleeding. Metabolic acidosis: often a consequence of shock, septic shock should be treated aggressively to avoid prolonged shock. In case of severe acidosis, pH < 7.2 and/or HCO3- < 15 mmol/L, or BE < -10, correction with bicarbonate is required. Immunoglobuline (IVIG) is effective in toxic shock syndrome or severe septic shock in a normal setting. dose 0.5g/kg/time IV.6. Continuous dialysis
Purpose: treatment of acute renal failure, removal of Cytokines and intermediate chemicals.Indication for continuous dialysis in case of acute renal failure with hemodynamic instability and one of the following criteria:
Electrolyte, acid-base disturbances that do not respond to medical therapy Fluid overload, no response to diuretics (>10% increase in baseline weight) Uremia syndrome
7. Surgery
Indication early surgical removal of pus, in severe cases both resuscitation and surgical intervention:Drainage of pus. Surgery to remove infection.

8. Follow up
Pulse, blood pressure, respiratory rate, consciousness, cyanosis, CRT every 15-30 minutes during shock resuscitation and then every 1-2 hours for the first 24 hours after shock release. Monitor urine output per hour, input/output/6-8 hours Monitor CVP, invasive arterial blood pressure, HATB – CVP, ScvO2 ≥ 70%, Lactate, lactate clearance, blood gas pH, HCO3, BE every hour for First 6 hours, 4-6 hours in the next 24 hours. Cardiac output, cardiac output index CI, SVV, SVR Tissue oxygen saturation SrO2/StO2 if available. Septic shock in children is a very serious and especially dangerous disease. This is a complication of a serious infection that, if not detected early and treated promptly, can be life-threatening. Diagnosis of shock and treatment of infection is difficult because there is no specific test to diagnose severe infection. Therefore, when the child has abnormal signs, parents need to quickly take the child to the doctor and treat.Vinmec International General Hospital is the address for receiving and examining respiratory diseases that infants and young children are susceptible to: viral fever, bacterial fever, respiratory infection, pneumonia in children and many diseases that require prompt emergency such as septic shock. With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.