This is an automatically translated article.
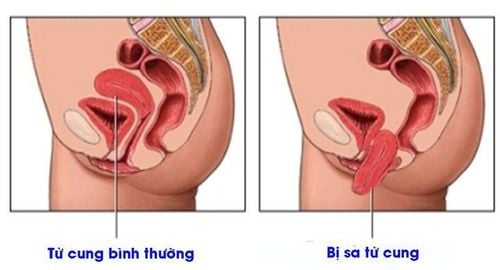
The article is expertly consulted by Master, Doctor Le Nhat Nguyen - Obstetrician-Gynecology Specialist - Vinmec Danang International General Hospital.Laparoscopic surgery for uterine prolapse is the first choice in the treatment of female genital prolapse with advantages such as: less pain, safety, fast recovery and limited recurrence, hospital stay time. Short term, reduced treatment costs, fewer complications, small surgical scars.
1. Treatment of genital prolapse
Genitourinary surgery is the common method of choice with complete hysterectomy with open or transvaginal laparoscopic surgery, vaginal and perineal reconstruction. There are many treatment methods for genital prolapse such as:Pelvic floor exercises, electrical stimulation of the muscles pessary ring (carrying) Vaginal surgery Hysterectomy/prostatectomy including surgery open or laparoscopic surgery. 1.1. Transvaginal genital prolapse surgery During vaginal surgery, the use of lifting mesh for bladder prolapse is better than using autologous tissue anatomically, there is no difference between lifting mesh and tissue functionally self. Lift nets increase the risk of complications (ulcers) so use of lift nets should be discussed on a case-by-case basis. In addition, do not enema before surgery.
Reconstruction or enhancement of the rectal septum are two techniques used for mid-rectal prolapse that will result in better anatomical results but the same functional outcome. Using undigested thread can lead to ulcers or granulomas so use slow gauge.
Sutures of the levator muscle lead to constipation in 50% of patients. Therefore, the levator muscle should not be sutured. Do not use an anterior rectal bio-lift. Synthetic lift nets need further evaluation. The rate of ulceration can be 5.6 - 12%, the rate of painful intercourse is about 63% (NP3). It is best not to specify a synthetic lifting mesh for rectal prolapse in the first place. Reconstruction of the posterior vaginal wall is recommended if the vagina is wide and the rectal prolapse is low. Systematic (AP) is not recommended.
In case of posterior vaginal wall or sacral prolapse, there is no difference between McCall and Richter method. Treatment of vaginal prolapse with the method of fixing protrusion through endoscopic and Richter, the anatomical results are the same but the difference is in pain after surgery. Outcomes are worse than the vaginal route.
Does hysterectomy change the anatomical and functional outcome of surgery for genital prolapse? Uterine and sacral ligament suspension is as effective as hysterectomy + apical suspension to the sacroiliac ligament but reduces hospital stay and early return to work. Cervical hypertrophy is a factor of recurrence. Cervical amputation is recommended if hypertrophy is present. Hysterectomy with a vaginal lift did not change the outcome compared with no hysterectomy.
If the protrusion is fixed, the hysterectomy will increase the surgical time and the blood loss will not reduce the risk of recurrence of the medial prolapse. Hysterectomy does not change sexual function. Uterine preservation does not change the risk of vaginal fistula if a vaginal lift is used. In the fixation of the protrusion process, if a hysterectomy is required, a partial hysterectomy is recommended because complete hysterectomy increases the risk of ulceration of the raised meshwork. There is no scientific evidence to perform a systematic hysterectomy in the treatment of Genital Prolapse

1.3 Laparoscopic surgery Laparoscopic surgery for uterine prolapse is the first choice in the treatment of female genital prolapse with advantages such as: less pain, safety, quick recovery and limited recurrence development, short hospital stay, reduced treatment costs, fewer complications, small surgical scars. Three-dimensional (3D) endoscopic technology is a modern means of assisting the surgeon to clearly observe anatomical landmarks (protrusion,...), the boundary of the cutting apex with the bladder, and stitches to fix the fascia. place. From there, surgery becomes safe, accurate, and improves treatment efficiency.
In particular, 3D laparoscopic surgery also brings many outstanding advantages in surgery such as: a larger operating theater, more clearly visible organs, helping to reduce the rate of complications in surgery. The success rate after laparoscopic suspensory surgery for genital prolapse is 96%, so this is a minimally invasive surgery and a new advancement that is initially being applied in the world, showing very good results. positive.

With outstanding advantages: Safety, minimizing the risk of complications and surgical infection, pain relief, less blood loss, fast recovery, ensuring aesthetics, the robot can be used for most cases requiring endoscopic treatment, especially in cancer treatment.
Doctor Le Nhat Nguyen has more than 20 years of experience in the field of Obstetrics and Gynecology. Formerly a doctor of obstetrics and gynecology at Gia Dinh People's Hospital in Ho Chi Minh City. BS has high expertise and strength in the diagnosis and treatment of Obstetrics and Gynecology diseases. Currently a Doctor of Obstetrics and Gynecology - Vinmec International Hospital Da Nang.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.