This is an automatically translated article.
Brachial plexus disease is a multifactorial disease that leads to damage, which can be acute or progressive. Among them, trauma is the most common cause. The following article will clarify some of the currently used brachial plexus treatment measures.
1. What is brachial plexus inflammation?
The brachial plexus (BRAY-key-el PLEK-sis) is a network of nerves that provide movement and sensation to the shoulder, arm, and hand. The brachial plexus is a nerve complex consisting of four cervical nerve roots (C5-C8) and the first thoracic nerve root (T1). These roots combine to form 3 stems. C5-C6 forms the upper body, C7 continues to be the mid-body, and C8-T1 forms the lower body.
Brachial plexitis is a neuromuscular atrophy caused by damage to the low motor neurons of the brachial plexus or some of its branches. The disease is uncommon and usually occurs in young people, presenting acutely with unilateral shoulder pain, flaccid paralysis of the shoulder muscles lasting a few days to a few weeks.
2. Symptoms of brachial plexitis
Clinical manifestations of brachial plexitis:
Motor paralysis of the muscles innervated by the brachial plexus nerves (examine each muscle group controlled by the terminal branches of the brachial plexus); Sensory paralysis caused by nerves of the brachial plexus (examine the sensory divisions of the nerves, in order from the supraclavicular region, shoulder, arm, forearm to hand); Horner's syndrome (ptosis, miosis, sunken eyes and dry eyes) is indicative of C8 and T1 rooting lesions; Sharp pain when percussion along the path of the brachial plexus in the supraclavicular region is a sign of root damage and the central coccyx is also in contact with the medulla. On the contrary, if it does not cause pain, it is more prone to uprooting lesions; Pain, burning, feeling of ants crawling, needles... are signs towards uprooting. Subclinical:
On conventional chest X-ray film, the damaged diaphragmatic arch is pulled higher than normal, a sign of phrenic nerve paralysis. This is contraindicated when using the phrenic nerve or the intercostal nerve as a donor. Magnetic Resonance Imaging (MRI): Pseudomeningoceles is a very valuable indirect diagnostic sign of the disease. CT film - myelography: Image of fibrosis in the origin of the nerve roots because they have been pulled out of the spinal cord. In addition, medullary pseudocysts in the spinal canal in addition to the dura mater are indirect signs of an uprooted lesion. The greatest value of CT - myelography is to allow the diagnosis of cases of root extraction without pseudocyst. Loss of nerve conduction on neuromuscular electricity. Signs and symptoms of brachial plexus injury can vary widely, depending on the severity and location of your injury. Usually only one arm is affected.
Damage to the brachial plexus can cause weakness or permanent disability. Even if the wound seems small, you may need medical attention. See your doctor if you have the following signs:
Weakness in your hand or arm; Neck pain; Symptoms in both arms.

Đám rối thần kinh cánh tay có thể khiến bạn yếu bàn tay hoặc cánh tay
3. Causes of brachial plexus inflammation
Injury to the upper nerves that form the brachial plexus tends to occur when your shoulder is pressed down while the neck is reaching up and away from the injured shoulder. The lower nerves are more likely to be injured when your arm is pressed overhead.
These injuries can occur in a number of ways, including:
Football players are stretched beyond their limit when they collide with other players. Difficult births predispose infants to brachial plexus injuries. Certain types of trauma such as a motor vehicle accident, motorcycle accident, fall, or gunshot wound. Tumors can grow in or along the brachial plexus, causing pressure on the brachial plexus or spreading to nerves. Radiation therapy to the chest can lead to brachial plexus damage.
4. Complications of brachial plexitis
Some injuries can cause temporary or permanent problems, such as:
Dryness and stiffness : If you have paralysis of your hand or arm, the joints can become stiff. This can make movement difficult. For that reason, your doctor will likely recommend ongoing physical therapy during your recovery. Pain: This leads to nerve damage and can become chronic. Arm numbness: If you lose feeling in your arm or hand, you're at risk for burns or injury without knowing it. Muscle weakness: Nerves grow back slowly and can take several years to heal after an injury. Permanent Disability: How well you recover from a serious brachial plexus injury depends on several factors, including your age and the type, location, and severity of the injury. Even with surgery, some people experience muscle weakness or permanent paralysis.
5. How to treat brachial plexus?
5.1. Medical treatment Patients are absolutely indicated for the cases of loss of nerve conduction due to blockage and relatively indicated for the case of axon rupture but the nerve sheath is still intact, especially in the internal tissue. Nerves are not severely damaged.
Medical treatment will include:
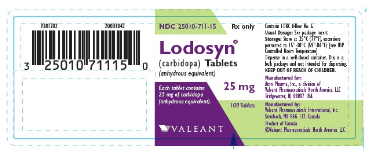
Taking vitamin B pills to enhance nerve regeneration (Methycobal, Nevramine); Physical therapy treatment to combat muscle atrophy, stiffness. 5.2. Surgical treatment 5.2 2.1. Injury to the superior roots (C5, C6, ±C7) Injury to nerve roots C5, C6 leads to loss of shoulder joint motion, elbow flexion due to paralysis of the superior scapular nerve, the deltoid and the musculoskeletal nerve. If C7 nerve root damage is associated, there is also decreased strength in some movements, such as elbow extension, thumb flexion, flexion and extension of the fingers, and decreased sensation in the palmar region (C7 nerve root). involved in <1% musculoskeletal, 6% ulnar nerve, 16% radial nerve, 19% median nerve), the following treatment is indicated:
In case of early arrival < 6 months: Transfer Nerve XI (or phrenic or intercostal nerve) feeds the superior scapular nerve and transfers the motor branch of the long head of the triceps to the anterior circumflex nerve to restore abduction and external rotation of the shoulder joint. Transfer 1 bundle of forearm motor fibers of the ulnar nerve to the brachial biceps nerve and transfer 1 bundle of forearm motor fibers to the brachial nerve to restore elbow flexion (Oberlin II, or dual nerve transfer). For cases of late treatment (>12 months): Tendon transfer surgery according to the method of Stendler A. 5.2 .2. Injury to the lower roots (C8, T1, ±C7) Injury to nerve roots C8, T1, ±C7 causes loss of motion in the neck - hand, there may be a few movements but very weak. Neurosurgery remains a challenge and there is no standard method. Some authors have used the XI nerve or the intercostal nerve or both to transfer the median nerve, but the results are very limited.
In the case of damage to a low root, the tendon of the musculoskeletal muscle will be selected with unimportant movements to make the tendon the driving force for tendon transfer surgery to restore more important movements. This needs to be based on each specific patient, there is currently no standard procedure.

Bác sĩ sau khi thăm khám sẽ đưa ra phương án điều trị đám rối thần kinh cánh tay tốt nhất
5.2 .3. Injury to the entire roots (C5, C6, C7, C8, T1) Injury to the entire roots will cause loss of movement and sensation of the extremities, from the base to the tip. This is a huge challenge for modern medicine and also a difficult problem because the nerve resources are limited while the neurorehabilitation requirements are very large. Currently, there are many trends with different purposes in the treatment of this lesion and there is no standard method. * Nerve source for:
Nerve XI: As a motor nerve, it has from 1,500 to 1,700 nerve fibers; The phrenic nerve: A motor nerve, originating from the C3 and C4 roots, and has about 800 nerve fibers; Intercostal nerve: As a mixed nerve, each intercostal nerve will have from 800 to 1,300 nerve fibers, in which the number of motor fibers is less than sensory fibers. Usually 3, 4, 5, and 6 intercostal nerves are used; Motor branch of deep cervical plexus: Each branch has 800 to 1,000 nerve fibers; The contralateral benign C7 root: It is a mixed motor and sensory nerve and has 27,213 ± 5417 nerve fibers (17,000 – 40,000). With the advantage of having a much higher number of nerve fibers than the nerves for the extra plexus on the same side of the lesion combined and leaving no significant sequelae after removal, the C7 root is also a reliable nerve source. * Nerve source:
Because of the limited nerve supply, priority should be given to restoring the nerves that govern important functions of the extremities in the following order: The musculoskeletal nerve is used to flex the elbow, the median nerve is to wrist-finger flexion and sensation in the hand region, the circumflex nerve for shoulder abduction. In addition, the receiving nerve will depend on the requirements and purposes of rehabilitation, which can be the radial nerve to extend the fingers, the superior scapular nerve to strengthen the shoulder abduction. * Source of graft nerve:
Commonly grafted nerves are sensory nerves, such as lateral saphenous nerve, brachial cutaneous nerve, medial brachial nerve. While, transferring the healthy C7 on the opposite side to the injured hand, the grafted nerve is the ulnar nerve with vascular supply to prevent fibrosis of the central nerve fibers. * Surgery to transfer the contralateral healthy C7 nerve root (<6 months and counting from the time of injury):
In the world: Transfer the healthy C7 nerve root to the paralyzed median nerve through a reversible ulnar nerve graft. There will be a continuous pedicle-like feeding vessel. Transfer of the C7 nerve root on the healthy side to the paralyzed median nerve through the ulnar ulnar graft in the free form. Transition of the lateral C7 nerve root through the anterior tunnel of the spine. Selective C7 nerve root transfer. In Vietnam: Transferring nerve XI to the superior scapular nerve supplying the supraspinal and subspinous muscles to restore abduction (may add enhanced phrenic nerve if bilateral phrenic nerve is normal). Transfer C7 from the healthy side to the sensory branch on the peripheral side of the thoracic cross-section, which is the ulnar nerve, which feeds the anterior deltoid branch, to enhance recovery of the abductor. The central end of the thoracic cross graft is the ulnar nerve, which feeds the musculoskeletal nerve to restore elbow flexion. Peripheral transposition of the thoracic cross section is the ulnar nerve that feeds the median nerve to restore wrist-finger flexion and hand sensation. Thus, compared with the existing literature, there are 3 technical changes in the transfer of the contralateral healthy C7 nerve root, which are:
Firstly, using the tunnel under the collarbone and between the base of the cervical fascia. anterior to the trachea instead of the previous graft tunnels. This is a shorter tunnel than the transthoracic subcutaneous tunnel; Simple and easy to perform without causing irritation like the retroesophageal line. Second, using two grafts, the ulnar nerve has a feeding vessel (due to the short tunnel) to transfer all the C7 nerve fibers on the healthy side to the receiving nerve on the injured side. Third, the two separate and vascular grafts are vascularized by the use of vascular sources in the central cephalic lamina and the ulnar nerve bundle is connected to the receiving region and simultaneously without resection of the medial ulnar nerve. When folded, cut to create 2 nerve endings connecting to 2 halves of C7 roots. * Functional free muscle transfer (over 12 months from the time of injury):
Because the target muscles have been fibrotic, there will be no indication for neurological intervention. At that time, functional free muscle transplantation will be indicated, the nerve for which is the XI nerve or the intercostal nerve. However, this method is often not as effective as neurointervention. Brachial plexitis is easy to be confused with other diseases with pain and limitation of shoulder movement such as: shoulder periarthritis, cervical spondylosis, acute scoliosis, cervical disc herniation. .. If not detected and treated early, often leave sequelae of muscle atrophy and limitation of movement, so patients with acute pain and weakness of shoulder muscles need to see a neurologist for diagnosis. and get treatment as soon as possible.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.