This is an automatically translated article.
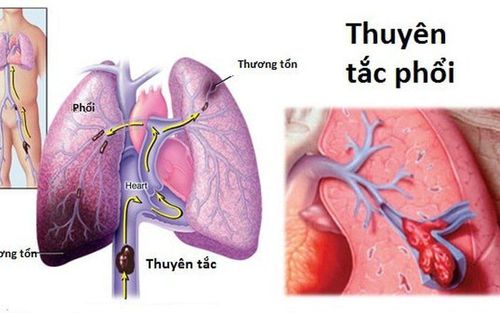
The article is professionally consulted by Master, Doctor Nguyen Huy Nhat - Respiratory Doctor - Department of Medical Examination & Internal Medicine - Vinmec Danang International General HospitalPulmonary embolism is a condition in which a blood clot enters a blood vessel in the lung, blocking the normal flow of blood in that area, interfering with air exchange, and can be life-threatening if left untreated. not detected and treated in time.
1. What is pulmonary embolism?
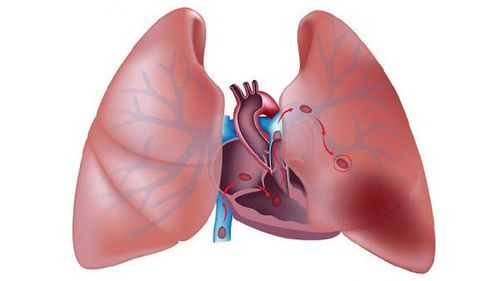
Normally, blood circulates through the lungs from the right heart to take in oxygen and get rid of carbon dioxide (gas exchange mechanism). The blood then circulates from the lungs back to the left heart to be pumped out to the rest of the body. Pulmonary embolism (PE) is a sudden blockage of a blood vessel in the lungs, blocking the normal flow of blood in that area, interfering with gas exchange. Acute pulmonary embolism occurs when blood clots that travel from other parts (especially the legs) to the lungs become blocked. Depending on the size of the clot and the number of blood vessels involved, a pulmonary embolism can be life-threatening and requires immediate treatment.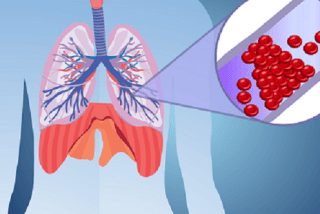
2. Diagnosis of pulmonary embolism
2.1 Clinical diagnosis First, the doctor will learn about the patient's symptoms, medical history and clinical examination to determine whether the patient has a pulmonary embolism or not. Warning symptoms of pulmonary embolism include:Shortness of breath, wheezing, often of sudden onset, shortness of breath both on exertion and at rest; Lightheadedness, chest pain, sharp pain when breathing in, heart palpitations; Low fever, loss of consciousness, coughing up blood. Clinical examination shows that the patient has tachypnea, tachycardia, pulmonary rales, decreased vocal cords, distended neck veins, swelling, redness, and pain in the lower extremities if accompanied by deep vein thrombosis.
2.2 Subclinical Diagnosis Laboratory methods that may be used to confirm the diagnosis of pulmonary embolism include:
Lower extremity vascular ultrasound: Lower extremity vein Doppler ultrasound is used to help the physician Can observe the flow of blood in the leg veins and the location of the blockage. This is a simple, non-invasive technique that can observe deep vein thrombosis. If a deep vein thrombosis is found, your doctor may suspect a pulmonary embolism as the cause of symptoms such as shortness of breath or chest pain. However, a negative ultrasound (no clot visible) does not rule out a deep vein thrombosis or pulmonary embolism because the clot may not be visible on the ultrasound screen. In this case, the doctor needs to perform other tests; Blood D-dimer test: Helps detect the breakdown product of a blood clot. If the blood level of D-dimer is high, it is more likely that there is a blood clot in the patient's vein and that is a warning sign of a pulmonary embolism. However, this test can still be positive in some situations, such as in patients who have recently had surgery or are pregnant. When the D-dimer test result is negative, there is a high probability that the patient does not have a deep vein thrombosis or pulmonary embolism. However, if the patient is at high risk of pulmonary embolism, the doctor suspects a blood clot, even if the D-dimer test is negative, the patient still needs to have other tests; Echocardiography of pulmonary embolism: A useful diagnostic method for cases of large embolism because ultrasound can help doctors see a large blood clot in the lungs or indirectly see its effect on the heart. . However, echocardiography is often difficult to detect small pulmonary embolisms; Lung scan: Also known as V/Q scan or ventilation/perfusion scan of the lungs, it is a specialized scanning method that helps doctors observe pulmonary circulation. This method is useful because it can give a fairly accurate result as to whether or not a pulmonary embolism is present. Lung scan is used in some special cases such as allergy to contrast agent used in CTPA, chronic kidney disease. However, this method is rarely applied, often replaced by MRI; CT scanner with multiple transducers with landscape (CTPA): A method of imaging the pulmonary blood vessels with contrast, helping the doctor to see the pulmonary arteries more clearly. CTPA is currently considered the noninvasive gold standard for the diagnosis of pulmonary embolism; Other routine tests: Other tests of the heart, lungs, and blood are often ordered to help diagnose disease or detect other conditions. Electrocardiogram (electrocardiogram or pulmonary embolism ECG), blood test, arterial blood gas test, chest X-ray,... are commonly used methods.

Acute myocardial infarction, especially right ventricular myocardial infarction; Acute left heart failure; Pericarditis , acute tamponade; Lobar pneumonia; Pneumothorax ; Broken ribs; Primary pulmonary hypertension; costochondritis; Bronchial asthma attacks ; Myalgia, intercostal neuralgia.
3. Treatment of pulmonary embolism
Treatment of pulmonary embolism due to blood clot is mainly anticoagulation and oxygen therapy in the early stages to improve dyspnea and hypoxemia. Specific treatment methods are:3.1 Use of anticoagulants Anticoagulants are also known as blood thinners. This medicine changes certain substances in the blood to prevent the formation of blood clots. However, it does not dissolve blood clots that have formed. Anticoagulants prevent blood clots in the lungs from becoming larger and prevent new blood clots from forming. Then, the body's self-repair mechanism will work to break down the clot on its own.
Anticoagulation therapy is usually started immediately after a pulmonary embolism is suspected to prevent disease progression while awaiting test results. Anticoagulants come in two forms: injection and oral tablet (or syrup for people who cannot swallow pills).
The injection form is standard heparin (unfractionated heparin) or low molecular weight heparin. Standard heparin, given intravenously (usually in the arm), is used for high-risk pulmonary embolism and in people with comorbidities such as chronic kidney disease. Low molecular weight heparin is injected under the skin of the abdomen. Low-molecular-weight heparin is also used in lower doses to prevent venous thromboembolism (pulmonary embolism and deep vein thrombosis) in some hospitalized patients, especially those already or undergoing major surgery). One drug, fondaparinux sodium, can also be given by injection in some cases to prevent venous thromboembolism or to treat pulmonary embolism or deep vein thrombosis. The pill or syrup used to prevent pulmonary embolism is warfarin, sintrom (acenocoumarol). In addition, some drugs with effects similar to warfarin such as rivaroxaban, apixaban can also be used to replace warfarin. Usually, injections are used at the beginning of treatment because they are effective immediately. After the injection and the diagnosis of pulmonary embolism, the patient may be prescribed oral warfarin. Warfarin usually takes a few days to take full effect.
Treatment of pulmonary embolism with anticoagulants is continued for up to 3 months in most cases. If the patient is at risk of re-embolization, the duration of treatment may be extended as prescribed by the doctor. For patients with pulmonary embolism during pregnancy, heparin injection will be preferred over warfarin because warfarin can cause birth defects in the fetus, especially during the first 3 months of pregnancy.

Oxygen inhalation to relieve shortness of breath; Intravenous fluids to support circulation; Close monitoring and intensive care if the patient is unwell or the pulmonary embolism is large. 3.3 Complementary therapies The following measures are used to treat large pulmonary embolism, patients who are very weak or unable to receive anticoagulation:
Thrombolysis: A drug that helps Dissolve the blood clot that has formed. The commonly used drug is Alteplase, which can be replaced by streptokinase or urokinase. It is stronger than the anticoagulants heparin and warfarin, but carries a higher risk of side effects such as bleeding in the brain; Using a inferior vena cava filter: A filter is placed in the inferior vena cava (the large vein that carries blood to the heart) to prevent blood clots from traveling to the lungs. This method is used in cases where anticoagulation alone does not effectively treat pulmonary embolism or the patient cannot take anticoagulation due to another medical problem; Embolectomy: As a last resort for patients with very severe pulmonary embolism, there is a high risk of death without surgery. In addition, patients who cannot take anticoagulants or thrombolytics because of the high risk of bleeding may also be offered surgical removal of the thrombus. This is a major surgery, carried out inside the chest, close to the heart and has a high risk of danger, so it requires an experienced doctor in a large hospital; Catheter embolectomy: This is done by threading a small catheter into a patient's blood vessel until it reaches the clot, so the doctor can remove the clot or break it up. clot with instruments inserted through the catheter. This is an intensive treatment that is only available in a few major hospitals. The prognosis of pulmonary embolism depends mainly on the type of pulmonary embolism and the presence of other comorbidities. With timely treatment, the prognosis is quite good and the patient can make a full recovery. After treatment for pulmonary embolism, patients should return for regular check-ups to monitor the progress of the disease, take medication as directed by the doctor, avoid lying down for too long or be inactive, do not smoke, do not wear tight clothes. monitoring, ... to treat the disease effectively, reduce the risk of disease aggravation or recurrence.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.