This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Gastrointestinal endoscopy is a method of screening and accurately detecting lesions occurring in the digestive tract that are difficult to detect with other diagnostic methods. Especially for ulcerative colitis with bleeding. The following article will help readers better understand the role of gastrointestinal endoscopy in the evaluation of bleeding ulcerative colitis.
1. Clinical manifestations of bleeding ulcerative colitis
Hemorrhagic ulcerative colitis is characterized by diffuse and superficial inflammatory lesions of the colonic mucosa, beginning in the rectum and extending to other segments of the colon. The small intestine is usually not involved, although the terminal ileum may have superficial inflammatory lesions. Based on the extent of colonic lesions, ulcerative colitis can be classified into the following types: Proctitis (localized lesions in the rectum), sigmoid colitis - rectum or left colon. (spread to the splenic angle) or diffuse/global colitis. The extent of the lesion is not only related to severity but also affects wages and treatment options. Symptoms and course of disease are related to the extent and severity of inflammatory lesions. Symptoms are often insidious, although the disease may develop acutely after an episode of infectious colitis or travel diarrhea. Proctitis causing bloody stools is the most common symptom of patients. The degree of bloody stools can be severe, profuse or moderate, bloody stools with mucus. The patient may have frequent urge to defecate and strain or increase the frequency of defecation. The more widespread the colonic lesion, the more severe the diarrhea, while if the patient is simply proctitis, the symptoms may alternate between episodes of constipation with episodes of bloody stools.
Abdominal pain before defecation or a feeling of abdominal distension will be encountered when the disease is advanced. In advanced or fulminant cases, the patient may present with systemic symptoms such as night sweats, fever, vomiting, nausea, weight loss accompanied by diarrhea. In addition, symptoms outside the gastrointestinal tract such as eyes, skin, joints, and liver may be experienced.

Proctitis is defined as localized inflammation in the rectum and is the mildest form of spread, accounting for 25-30% of cases at diagnosis. Patients often have bloody stools, a feeling of needing to defecate or sometimes constipation due to slow stool movement in the right colon. Systemic symptoms are rare, but concomitant skin or joint involvement may be seen. Approximately 30-40% of patients with ulcerative proctitis then progress to other segments of the colon. Ulcerative sigmoid colitis - also known as left colitis occurs in 40% of cases, patients may have symptoms alternating between constipation and diarrhea accompanied by abdominal pain, nausea. , bloody stools. Left iliac fossa colic and extra-gastrointestinal symptoms were more common than those with ulcerative proctitis alone.
Ulcerative colitis is diagnosed when the inflammatory lesion extends as far as the transverse colon or the right colon. Patients often present with diarrhea, bloody stools, painful defecation, abdominal fullness, abdominal cramps or localized pain. In addition, patients in this group often have weight loss, systemic symptoms, extra-gastrointestinal symptoms, and anemia. Toxic megacolon is the most severe complication of hemorrhagic ulcerative colitis when the inflammatory lesion spreads from the superficial mucosa to the submucosal and muscular layers. This complication often occurs in patients with disseminated colitis or severe colitis. Clinical manifestations include fever, exhaustion, severe abdominal cramps, abdominal distention, and local or total abdominal pain.
2. 2. The role of gastrointestinal endoscopy in the evaluation of bleeding ulcerative colitis
2.1. Colonoscopy 2.1.1. Indications The ECCO 2017 Guidelines recommend colonoscopy with examination of intra-ileal lesions as an exploratory method to confirm the diagnosis of IBD pathologies. In hemorrhagic ulcerative colitis, the initial endoscopic lesion is in the rectal region proximal to the anal canal. Then, gradually spread upwards with a continuous, concentric nature. The boundary between the lesion and the normal mucosa is clear. Occasionally, a regional lesion in the cecum or no lesion in the rectum may be seen necessitating an evaluation of the small bowel lesion. As in Crohn's, to accurately evaluate the lesion for hemorrhagic ulcerative colitis, multiple biopsies from the terminal ileum and five segments of the colon (upper, transverse, descending colon) are required. sigmoid colon, rectum). Ideally, each biopsies should include two sections of the normal mucosa and the lesion. When endoscopic and histopathological results are not clear, colonoscopy with biopsies can be performed in combination with other investigations such as upper gastrointestinal endoscopy if the patient is symptomatic, capsule endoscopy. or colonoscopy. For cases where the disease recurs, is resistant to treatment, appears with new symptoms, or considers surgery, it is necessary to re-evaluate the extent of the damage endoscopically.

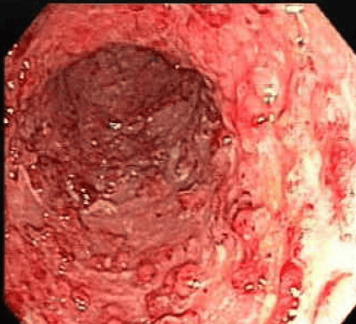
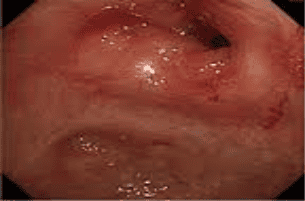
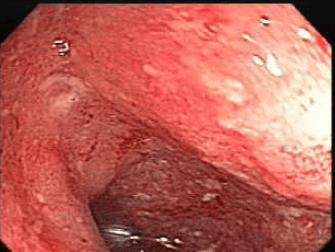
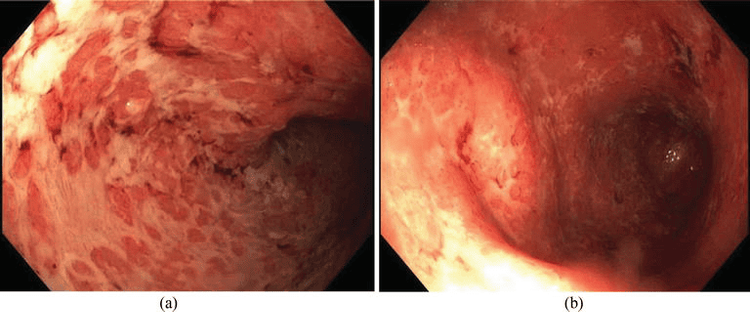
2.1.2. Evaluation of lesions The endoscopic image of bleeding ulcerative colitis is quite diverse depending on the stage of disease progression and extent of lesions. Typical features include:
Loss of the normal capillary network: When compared with the normal colonic mucosa, the capillary network in the affected area is unknown and unevenly distributed in the early stages of the process. inflammation. As the disease progresses, the normal capillary network image will be lost. Mucosal Congestion: Ranging from mild congestion to dilated all blood vessels in the mucosa. The oesophageal mucosa is contrasted with the soft mucosa of the normal colon. Mucosal edema: In the acute stage of inflammation, mucosal edema and sometimes, if much edema, can cause narrowing of the colonic lumen but not a true stricture.
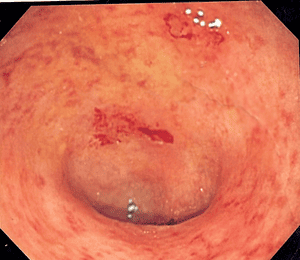
Bleeding easily: When touching the lamp or inflating, it is easy to bleed, sometimes it is observed that the mucosa is self-bleeding.

Exudation: Mucosal secretions are abundant and this condition worsens with the degree of inflammation of the mucosa. True bleeding: From the inflamed mucosa, bleeding is seen. In cases of heavy bleeding, it is difficult to determine the bleeding point.
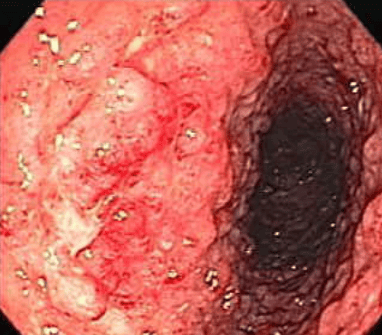
Ulcers: Small, superficial ulcers. In severe cases, deep and extensive ulcers of various sizes and shapes can be seen. Occasionally, long ulcerations such as those in Crohn's or lithiasis may be seen if there are long-standing ulcers. However, the mucosa surrounding the ulcer has a different nature. Peri-ulcer mucosa in Crohn's patients was normal, while in patients with ulcerative colitis bleeding, the mucosa was congested, rough, and lost the capillary network. Thus, the ulcerative characteristic of Crohn's as a "simple ulcer" is different from the "inflammatory ulcer" characteristic of hemorrhagic ulcerative colitis.

In mild cases of inflammation, when recovered, the colonic mucosa returns to an almost normal image and it will be difficult to distinguish the boundary between the area with and without previous lesions. However, for cases of moderate to severe inflammation, when the mucosa of the damaged area regenerates and heals, it is possible to see the old scar image, the image of a pseudo-diverticulum due to the contraction of the large scars, mucosal bridges. As the disease progresses over a long period of time, the colonic mucosa may lose its normal folds, narrow the colonic lumen, or post-inflammatory pseudopolyposis lesions. When a narrow lesion is present, a biopsy should be performed to rule out malignancy.

2.1.3. Assessment of lesion location In the Montreal classification, based on the location of the lesion, it will be divided into: Injuries in the rectum, lesions in the left colon and extensive lesions. Over time, the distribution of lesions may change, often tending to spread from the rectum to the upper colon. One study has noted that 28% of cases after 10 years will have a more extensive lesion progression than the initial one. Internal lesion/colon bleeding according to the Montreal classification:
| Thuật ngữ | Mức độ | Mô tả |
| E1 | Viêm trực tràng | Tổn thương khu trú ở trực tràng, vị trí đầu trên tổn thương là vùng nối trực tràng - đại tràng sigma |
| E2 | Viêm đại tràng trái | Tổn thương đại tràng lan đến góc lách |
| E3 | Lan tỏa | Tổn thương qua đại tràng góc lách, bao gồm cả những trường hợp viêm toàn bộ đại tràng |
In addition, in bleeding ulcerative colitis, there are two other types of lesions:
Retrograde ileitis: This is a term used on both endoscopy and histopathology to refer to a continuous inflammatory lesion, spreading from the cecum to the terminal ileum, commonly seen in ulcerative colitis with extensive bleeding. Inflammatory lesions of the right colon and terminal ileum were morphologically similar to those of other segments of the colon and the ileocecal valve was clearly observed. It can be distinguished from ileal lesions in Crohn's by the absence of stenotic lesions, the absence of ileocecal or intra-ileal valve ulcers. Retrograde ileitis is common in hemorrhagic ulcerative colitis patients presenting with primary sclerosing cholangitis and is detected in 10-20% of the total colectomy specimens. in the group of patients with extensive lesions. The group of patients with bleeding ulcerative colitis with ileal lesions tended to be more difficult to treat and required earlier surgery.
Localized inflammation in the cecum or around the appendix: Features of intermittent inflammatory lesions with the remaining mucosal areas of the colon. In particular, no lesions were found in other segments of the right colon.
2.1.4. Classification of severity of ulcerative colitis lesions on endoscopic bleeding was first mentioned by two authors Truelove and Witts in 1955 in a placebo-controlled trial to evaluate the effect of cortisone in the treatment of disease in the active stage. According to mucosal changes, divided into three types: 1 - normal or near normal (slightly congested or mildly rough), 2 - with improvement, 3 - no improvement or worsening. However, the disadvantage of this classification is that the lesions are not clearly defined.
By 1964, Baron et al evaluated the consensus among endoscopists in the description of lesions in 60 patients with bleeding ulcerative colitis undergoing sigmoidoscopy using a new scale. This scale is based on the severity of bleeding and does not take into account the presence of ulcerative lesions. Next, the St Mark index was born to evaluate the severity of mucosal inflammation from 0 to 2, also mainly focusing on evaluating mucosal bleeding. Later, more scales and indexes were used to assess endoscopic severity more fully and were mainly born from clinical trials evaluating the effectiveness of therapeutic drugs:
The UC-DAI index was developed in a placebo-controlled trial to evaluate the effectiveness of mesalamine enemas based on three factors: mucosal vulnerability, excessive exudation, and spontaneous bleeding. Mayo Scale: Developed in 1987 based on a placebo-controlled trial to assess the effectiveness of oral delayed-release mesalamine. Inflammation of the rectal mucosa on endoscopy was evaluated according to four levels from 0 to 3 based on three imaging factors, the image of blood vessels and the degree of bleeding of the mucosa. One of the disadvantages of the above indicators and scales is that the definition of treatment response or recovery on endoscopic images is not recognized. To develop a recognized assessment tool, the UCEIS index was born with the main criteria: Vascular morphology, bleeding and ulceration. The advantage of this index is that there is a clear definition of the levels and the remarkable point in this indicator is the removal of the bleeding mucosal factor.
2.2. Upper GI endoscopy Upper gastrointestinal tract lesions in bleeding ulcerative colitis are uncommon. Therefore, the indication for upper gastrointestinal endoscopy is made when the patient has symptoms. Several reports have documented upper gastrointestinal tract lesions in patients with bleeding ulcerative colitis. However, the criteria for diagnosing upper gastrointestinal lesions associated with ulcerative colitis have not been agreed to date.
Currently, Vinmec International General Hospital is being equipped with the most modern gastrointestinal endoscopy equipment of Olympus with the method of endoscopy with narrow band of light (NBI). This is a breakthrough method in screening and diagnosing cancers of the gastrointestinal tract (esophagus, stomach, duodenum and colon and rectum) at early and very early stages. NBI endoscopic images have high resolution and resolution, so it is easy for doctors to detect small changes in color, morphology of cancerous and precancerous lesions that are difficult to detect with conventional endoscopy. .
Along with modern machinery system, when endoscopy of esophagus, stomach, duodenum combined with biopsies at Vinmec, patients are performed by a team of good specialists such as:
Doctor, Doctor Bui Xuan Truong - Doctor of General Internal Medicine - Vinmec Times City International Hospital, with 20 years of experience in the field of Gastroenterology - Hepatobiliary - Hepatitis - Gastrointestinal endoscopy and Gastrointestinal ultrasound.
Doctor Bui Thu Huong - Pediatric Center - Vinmec Times City International Hospital, with 37 years of experience in the industry, former Head of Gastroenterology Department - National Children's Hospital.
In addition, colorectal endoscopy and all other technical procedures performed at Vinmec are strictly controlled, meeting international quality standards, ensuring safety and quality for patients.
Before each operation, the endoscope system is guaranteed to be sterile, bringing absolute safety to the patient. After the procedure is over, the endoscope is cleaned with an automatic Olympus endoscope washing machine under the RO water purification system.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.