This is an automatically translated article.
Posted by Master, Doctor Tran Quynh Trang - Doctor of Biochemistry Laboratory - Laboratory Department - Vinmec Times City International Hospital
Tg and antiTg tests are not used to diagnose thyroid cancer, this test is only valid for monitoring the disease after treatment for well-differentiated thyroid cancer.
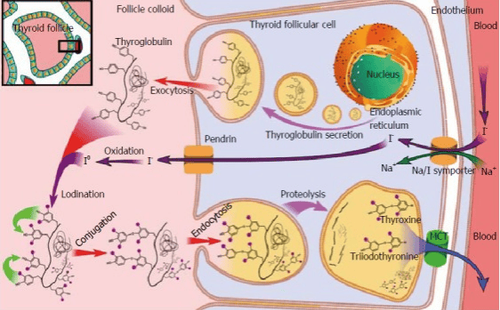
Thyroglobulin (TG) is a glycoprotein molecule produced exclusively by thyroid follicular cells. They are stored as colloid in the thyroid capsule, iodized, and broken down to T4 (Thyroxine) and T3 (Triiodothyronine). The thyroid gland produces the hormones T4 (Thyroxine) and T3 (Triiodothyronine) that help regulate the body's use of energy. It is a small butterfly-shaped organ located at the front of the neck and is made up of very small, ball-shaped structures called cysts that produce and store thyroglobulin.
Thyroglobulin plays a decisive role in the synthesis of thyroid hormones T3 and T4. The production of these hormones and their release into the bloodstream is stimulated by the hormone TSH) of the pituitary gland.
Thyroglobulin is produced in all healthy people and its blood levels are normal. Thyroglobulin levels are increased in non-cancerous patients (Graves disease, subacute thyroiditis, Hashimoto's thyroiditis) and thyroid cancer patients. Therefore, it is on the one hand a nonspecific marker of thyroid dysfunction and on the other hand a tumor marker that can be used to monitor patients with papillary and follicular thyroid cancer after diagnosis. . Tumor markers are substances made by cancer cells or normal cells in response to cancer in the body.
The TG test may be used in conjunction with the TSH test, prior to thyroid cancer treatment, to determine if cancer cells are producing thyroglobulin. Thyroglobulin tests may be ordered at intervals after treatment to monitor for recurrence of the cancer. Because serum thyroglobulin levels are proportional to thyroid tissue volume, it can be used to assess the severity of cancer at presentation.
Thyroglobulin in serum has a half-life of 65 h. The serum thyroglobulin concentration is proportional to the volume of thyroid tissue in the body with a concentration of 1 ng/mL per 1 g of thyroid mass. Since the size of a normal thyroid is 20-25 g, the reference range should generally be around 20 to 25 ng/mL. However, serum thyroglobulin concentrations are dependent on the sex and dietary intake of the patient. In iodine-deficient countries, the reference range may be higher. This is because the serum TSH is elevated in the presence of iodine deficiency, which stimulates the follicular cells to synthesize more thyroglobulin. In addition to gender and iodine intake, measured thyroglobulin levels are influenced by anti-thyroglobulin (anti-TG) autoantibodies, smoking, and TSH status unrelated to iodine intake. The measured serum thyroglobulin concentration is masked by the presence of anti-TG in the blood.
Anti-TGAb binds to thyroglobulin molecules that mask the epithelium on the thyroglobulin molecule to which radioimmunoassay (RIA) antibodies bind. As a result, Thyroglobulin levels, as measured by RIA in these patients, will be artificially low. Anti-TG may be elevated in Hashimoto's disease, Graves' disease, 20% of thyroid carcinoma patients, and 10% of the general population without any thyroid disease. Thyroglobulin testing is also indicated to help differentiate between subacute thyroiditis and thyrotoxicosis , helping to determine the cause of congenital hypothyroidism in the newborn . It is also ordered for the length of time you are taking antithyroid drugs (Graves' disease) to determine response to treatment.
Postoperative serum thyroglobulin levels reflect residual thyroid mass. In the absence of metastatic disease, this reflects the size of the thyroid gland left over during surgery. Since Thyroglobulin has a half-life of close to 3 days, it can be shown that the Thyroglobulin level should be less than 0.5 ng/mL by the end of the third week after total or near total thyroidectomy for tumors of this size. three times the normal size. This can be used as a guide to initiating radioactive iodine therapy to remove residual, residual thyroid mass as a result of inadequate surgery or metastatic disease. However, although such a hypothesis carries a high positive predictive value, a negative result does not reliably rule out residual disease. The serum thyroglobulin concentration at the 3rd week of surgery depends not only on the residual thyroid mass, but also on the size of the gland at the time of surgery as well as on the tumor's ability to produce Thyroglobulin.

Thyroglobulin can be secreted by differentiated cancer cells of the thyroid gland. This includes nearly two-thirds of differentiated thyroid cancers (cysts, all papillary carcinomas, Hurthle cell tumors of the thyroid), up to 50% of thyroid cancers. poorly differentiated and non-productive and some medullary cancers. Cancerous tissues can be stained with immunohistochemical methods for specific demonstration of Thyroglobulin. Thyroglobulin has been demonstrated in cancerous cysts in both the thyroid as well as in metastatic deposits in the lymph nodes and elsewhere.
The use of Thyroglobulin as a screening and diagnostic tool for differentiated thyroid cancer is poor (Sensitivity and specificity of 70% and 80% for follicular carcinoma, respectively) because both the Both benign and malignant thyroid glands secrete Thyroglobulin. Elevated Thyroglobulin levels can be seen in benign conditions such as Graves' disease and thyroiditis, as well as in thyroid cancer. Furthermore, there is a subgroup of thyroid cancer patients (12%) with low thyroglobulin levels as opposed to a minority with very high blood levels (>1000 ng/mL). Levels > 5000 ng/mL are indicative of metastatic disease.
People with high serum Thyroglobulin levels after thyroidectomy are more likely to have cancer recurrence, which is proportional to the likelihood of residual metastasis. However, high serum thyroglobulin can be caused by distant metastatic disease or incomplete removal of the thyroid gland during thyroidectomy. Holsinger et al. reported that 57% of patients presumed to have had a total thyroidectomy for thyroid cancer had residual thyroid tissue when examined with a postoperative radioactive iodine uptake test. Therefore, the surgeon must make sure that the entire thyroid gland is removed before using Thyroglobulin as a prognostic indicator. Or else, the patient must undergo radioactive iodine resection before the Thyroglobulin test.
Thyroglobulin has been used routinely to monitor disease recurrence after thyroidectomy. Not only the first relapse but also subsequent relapses can be detected by monitoring serum Thyroglobulin levels. Thyroglobulin levels must be taken every 6 to 12 months. However, certain points should be kept in mind when using Thyroglobulin only as a tumor marker to detect recurrence.
Normal value: 1.4 – 78 ng/mL.
Thyrogobulin concentration increases in the following cases:
Thyroid cancer Benign thyroid tumor. Most benign (noncancerous) thyroid tumors are capable of producing thyroglobulin. Thyroid nodules: Nodules are areas of tissue or cysts under the skin. Most nodules are benign, but a small percentage are cancerous. Underactive thyroid: Most people with an underactive thyroid gland have high levels of TSH, which increases thyroglobulin production. Graves' disease is an autoimmune disease that causes the thyroid gland to become overactive. Iodine deficiency and excess: An iodine deficiency causes the body to secrete more TSH, the thyroid gland produces more thyroglobulin. Taking too much iodine can also increase thyroglobulin levels. Too much iodine reduces the release of thyroid hormone, which increases TSH and thyroglobulin levels. Cirrhosis, hepatitis or nonalcoholic fatty liver disease. In a study of 134 people, people with cirrhosis had 84% higher thyroglobulin levels than healthy controls. Acromegaly: Acromegaly is a disorder caused by overproduction of growth hormone from the pituitary gland. People with acromegaly have an enlarged thyroid gland that produces higher amounts of thyroglobulin. Medications: The following medicines can increase thyroglobulin levels: Medicines used to treat an overactive thyroid, such as Methimazole (Tapazole) and Carbimazole (Neo-mercazole). Amiodarone (Nexterone, Pacerone), an iodine-containing medicine used to treat arrhythmias. Thyroglobulin levels decrease in the following cases:
Synthetic T4 hormone: Thyrotoxicosis (TF: factitia) is a condition caused by taking too much of the synthetic hormone T4 (levothyroxine). Thyroglobulin levels are very low or undetectable in people with this condition. Thyroidectomy: Thyroglobulin is made only in the thyroid gland or by thyroid cancer cells. This means that people without a thyroid gland will have undetectable levels of thyroglobulin. Medications: The following medicines can lower thyroglobulin levels: Levothyroxine, Synthetic TSH (Thyrogen), Prednisolone...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
1. Yalcin S, Ulger BV, Parlak O, Ucar AE, Sarikaya SM, Ozer M, Korukluoglu B, Yalcin B, Kusdemir A. The role of preoperative serum thyroglobulin and thyroid auto-antibody levels before histopathological diagnosis of thyroid cancers. Turk J Med Sci. 2011;41:487–493. [Google Scholar]
2. Hocevar M, Auersperg M, Stanovnik L. The dynamics of serum thyroglobulin elimination from the body after thyroid surgery. Eur J Surg Oncol. 1997;23:208–210. [PubMed] [Google Scholar]
3. Giovanella L, Imperiali M, Ferrari A, Palumbo A, Furlani L, Graziani MS, Castello R. Serum thyroglobulin reference values according to NACB criteria in healthy subjects with normal thyroid ultrasound. Clin Chem Lab Med. 2012;50:891–893. [PubMed] [Google Scholar]
4. Ovadia YS, Gefel D, Turkot S, Aharoni D, Fytlovich S, Troen AM. Elevated Serum Thyroglobulin and Low Iodine Intake Are Associated with Nontoxic Nodular Goiter among Adults Living near the Eastern Mediterranean Coast. J Thyroid Res. 2014;2014:913672. [PMC free article] [PubMed] [Google Scholar]