This is an automatically translated article.
The temporomandibular joint (TMJ) has the same operating principle as a sliding hinge, helping to connect the jawbone with the skull. Temporomandibular joint disorder (TMD) causes pain in the temporomandibular joint and the muscles that control jaw movement.1. What is temporomandibular joint disorder?
The cause of temporomandibular joint disorder is still not exactly determined. TMD pain can be the result of a combination of factors such as genetic factors, arthritis, or trauma to the jaw area. Some patients with temporomandibular joint disorders may have a tendency to frequently grind their teeth, but this does not mean that someone with a habit of grinding their teeth will cause TMJ.
In most cases, TMD-related temporomandibular pain is temporary and can be relieved with appropriate care or conservative treatment. Surgery is often indicated last when conservative measures are ineffective, but some patients with temporomandibular joint disorders may benefit from this treatment.
2. Signs suggestive of temporomandibular joint disorder
Common symptoms of this syndrome include:
Pain in the position of the jawbone; Temporomandibular pain on 1 or both sides; Pain in and around the ear; Difficulty chewing or pain when chewing; Pain in the entire face; Stuck or locked temporomandibular joint, the patient has difficulty opening or closing the mouth; A clicking sound occurs when you open your mouth or chew; Sudden difficulty chewing or biting, discomfort when the upper and lower teeth do not match; Swelling on one side of the face; In addition, people with TMJ may experience toothache, headache, neck pain, dizziness, hearing problems, shoulder pain, and ringing in the ears.
3. Causes of temporomandibular joint disorders
The temporomandibular joint acts as a sliding hinge. The bones of the temporomandibular joint can move smoothly because they are covered by cartilage and are separated by a small disc (which absorbs force).
Common causes of TMD are injuries to the jaw, joints, or muscles of the head and neck. Besides, there are other causes of temporomandibular joint disorder including:
Habit of grinding teeth inadvertently creating a lot of pressure on joints; Abnormal movement between the condyle of the jaw and the disc portion of the temporomandibular joint; Arthritis, cartilage damage; Nervous tension leads to facial muscle tension or teeth grinding; The part of the temporal disc that is eroded or moved out of its normal topology. However, there are many cases where the cause of temporomandibular joint disorder is not clear.
Thói quen nghiến răng là một trong các nguyên nhân gây rối loạn khớp thái dương hàm
4. Diagnosis of temporomandibular joint disorder syndrome
Many other conditions can cause symptoms similar to TMD such as tooth decay, gum disease, problems related to the facial sinuses or arthritis. To determine exactly, the doctor will discuss with the patient about the medical history and then perform the appropriate examination measures.
The doctor will examine the condition of the temporomandibular joint and ask if the patient has signs of temporomandibular pain, listen to a click or a sound similar to grinding teeth when the joint moves. At the same time, the doctor needs to record the jawbone activity and check for locking or jamming when the patient opens or closes the mouth. In addition, the doctor will check for possible biting and problems with the muscles of the face.
Some imaging methods help diagnose temporomandibular joint disorders:
Facial X-ray helps to observe the condition of jaw bone, temporomandibular joint and teeth; Magnetic resonance imaging: The image on the MRI film helps to detect whether the temporomandibular disc is in the correct position when the jawbone moves or not; Computed tomography (CT) scan to document the bones of the temporomandibular joint.
5. Home remedies for temporomandibular joint disorders
Patients can apply home remedies to relieve TMD symptoms under the guidance of a doctor, including:
Using over-the-counter drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) to relieve symptoms muscle swelling and pain; Cold compress: The patient uses an ice pack to apply on the side of the face with pain in the temples for 10 minutes; Do a few simple jaw stretches. Then apply a warm towel for 5 minutes; Eat soft foods, add yogurt, mashed potatoes, cheese, soups, eggs, fish, fruits, cooked vegetables, beans and whole grains to your daily menu. When processing, food should be cut into small pieces to limit chewing. Minimize foods that are too hard, crunchy, chewy or foods that are too thick and require opening the mouth wide; Limit jaw movement, yawning and chewing continuously. Be careful not to scream, sing, or do anything that causes your mouth to open wide; Do not rest your chin on your hand or hold the phone between your shoulder and ear; Try to keep your teeth apart to reduce pressure on the jawbone. Patients with temporomandibular joint disorder can control bruxism by placing the tongue between the two teeth; Watch now: Jaw fatigue, ear pain: Is it a temporomandibular disorder?
6. Methods of treatment of temporomandibular joint disorder syndrome
Treatment measures for temporomandibular joint disorder have been studied, including:
Treatment with drugs:
high-dose NSAIDs when patients have temporal pain and swelling; Muscle relaxants: Has the effect of relaxing the jawbone if the patient grinds his teeth continuously; Anti-anxiety drugs: Effective in reducing stress, a risk factor for temporomandibular joint syndrome. Especially in low doses, anti-anxiety medications can help control or relieve mild pain; Note that muscle relaxants and anti-anxiety medications are available by prescription only. Night Protection Brace: This plastic appliance fits snugly over the upper and lower teeth and is responsible for keeping them from touching each other. Thus, limiting teeth grinding and also helping to correct the bite by adjusting the teeth into the correct position.
Orthodontics: Dentists can replace missing teeth and use braces to balance the bite surface of the teeth or to correct problems in the bite.
Other treatments:
Transcutaneous electrical nerve stimulation (TENS): This therapy uses low-intensity electrical currents to stimulate and thereby relieve pain caused by the TMJ and facial muscles. relax. This TMJ disorder intervention can be done at the clinic or at home; Ultrasound: Using ultrasound waves to impact joints to relieve pain or improve mobility; Injected into the trigger point: This uses pain relievers or anesthetics to be injected into the muscles (also called "trigger points") to relieve pain; Therapy uses radio waves to stimulate joints, thereby increasing blood flow and reducing pain; Low-frequency laser therapy: This therapy can help reduce pain, reduce inflammation, and help you move your neck more freely and open your mouth wider.

Điều trị nội khoa được bác sĩ lựa chọn trong điều trị rối loạn khớp thái dương hàm
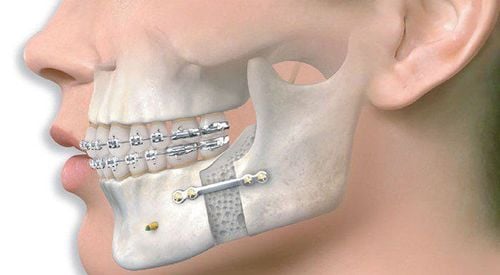
7. Temporomandibular joint surgery
Surgery for temporomandibular joint disorder should be considered when other treatments are not effective. However, the results of surgery will not be changed, so the patient needs to consider, consult and discuss with the doctor carefully before performing.
Currently, there are 3 surgical techniques for temporomandibular joint disorder and the choice depends on the patient's condition:
Arthroscopy: Indicated when the patient has no history of disease related to the temporomandibular joint function but the match is locked. The doctor will anesthetize the patient, then insert the needle into the temporomandibular joint and rinse it. In addition, the doctor may use a special instrument to remove damaged tissue or remove the temporal disc stuck in the joint.
Arthroscopy: This method uses an arthroscope that allows the doctor to see inside the temporomandibular joint. The patient needs to be under general anesthesia, then the doctor makes a small incision in front of the ear and inserts the endoscope. The endoscope is connected to a monitor so the doctor can examine the joint and surrounding areas. During that process, the doctor may remove inflammatory tissue or rearrange the structures of the joint. Arthroscopy is a minimally invasive surgery with minimal scarring, fewer complications, and a faster recovery time than an open surgery.
Arthroscopy: Depending on the cause of the TMJ and when arthroscopy is not possible. The patient may be indicated for open joint surgery if the following conditions are present:
The bone structures in the temporomandibular joint are being worn down; A lump in or around a joint; The temporomandibular joint is scarred or has bone fragments; The patient needs to be under general anesthesia, then the doctor will surgically open the entire area around the joint for full view and better access. Patients will need more time to recover from open surgery, the possibility of scarring or nerve damage is higher.
With many years of experience in the examination and treatment of oral and maxillofacial diseases, now Vinmec International General Hospital has become one of the major health care centers, capable of examining and screening filtering and treating many diseases in depth. Therefore, if there are signs of temporomandibular joint disorder, you can go to Vinmec International General Hospital to examine and receive support and advice from doctors and health experts.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference sources: mayoclinic.org, webmd.com