This is an automatically translated article.
Acute lymphoblastic leukemia (ALL) is the most common childhood cancer, usually occurring in children aged 1-4 years. Currently, the rate of successful treatment for leukemia is increasing, especially the survival rate in children with acute lymphoblastic leukemia (ALL) is improving positively.
1. Factors that increase the risk of acute lymphoblastic leukemia (ALL)
A risk factor is any factor that increases a person's chance of getting cancer. Although cancer risk factors often affect the likelihood of getting cancer, most do not directly cause cancer. Some people have several risk factors but do not get cancer, while others have no risk factors for cancer.
Although doctors have not found the main cause of leukemia in children, there is some evidence that genetic factors play a role in acute lymphoblastic leukemia (ALL):
Children born with genetic or immune system disorders, such as Down syndrome, ataxia telangiectasia, and Bloom's syndrome may have a higher risk of developing leukemia. One of the twins has ALL before the age of 6, the other has a high risk of leukemia. If one of the twins has leukemia in the first few months of life, the other will always have the same type of leukemia.
Bệnh bạch cầu cấp dòng Lympho (ALL)
2. Treatment of acute lymphoblastic leukemia in children
Doctors will best plan the treatment of acute lymphoblastic leukemia in children based on the following factors:
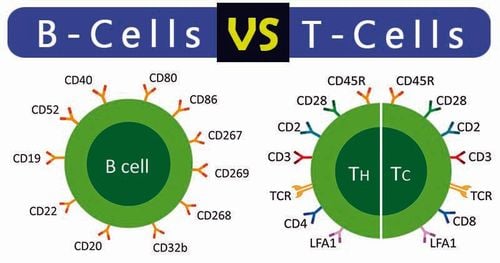
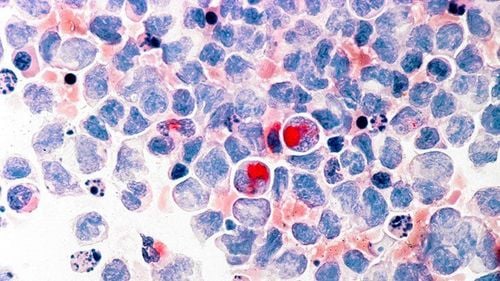
Age . Infants under 12 months of age and children 10 years of age and older require more intensive treatment. WBC count. Children with very high white blood cell counts need more intensive treatment. Normally, white blood cell counts are considered very high if they are more than 50,000 per microliter (ml). Immunology. This test shows the types and amounts of proteins made or expressed by the leukemia cells. Knowing whether cancer cells express the same proteins as normal white blood cells called B cells or T cells will help doctors plan appropriate treatment. It is also useful to help predict how treatment will work. Genetic abnormalities in white blood cells. Abnormal chromosome counts, abnormal structural changes in chromosomes, or certain molecular genetic changes in the chromosomes of leukemia cells can affect outcome and treatment. Note that the genetic changes mentioned here are changes in the genes of the leukemia cells, not the children's cells - most children with leukemia have completely normal genes. often. Early treatment response. How well treatment is done during the first 1 to 4 weeks of treatment can predict the overall response of leukemia to treatment. This will be determined by checking the child's blood or bone marrow regularly. Recent studies have shown that some children need stronger treatment to improve their chances of a cure. This includes children whose cancer does not respond well to early treatment or who have high levels of residual leukemia cells (cells left after treatment) at the end of treatment. remission process.
3. Survival in children with acute lymphoblastic leukemia (ALL)
After active cancer treatment is over, children and their families may experience a mixture of feelings that can become stronger, including joy, care, relief, guilt and fear. Some people say they appreciate life more after a cancer diagnosis. Other families are very worried about their child's health and are unsure about dealing with daily life.Stress can arise from frequent inquiries about health care that ends after treatment is completed. Often, the emotions of caregivers of sick children can provide a sense of security during treatment in children and their families. This can be especially true when new worries and challenges emerge over time, such as any late effects of treatment, educational problems, emotions, sexual development, and concerns. fertility, or financial problems.

Sau điều trị ung thư, trẻ cần được quan tâm đến xúc cảm
Each family faces different concerns and challenges. With any challenge, a good first step is to be able to recognize each fear and talk about it. Coping effectively requires:
Understanding the challenge your family is facing Thinking through solutions Asking for and allowing the support of others Feeling comfortable with the course of action your family chooses . It can be helpful to join an in-person support group or online community of childhood cancer survivors. Support groups also create connections for parents of children diagnosed with cancer. This allows you to talk to people who have had similar experiences. Other options for finding support include talking to a friend or member of the health care team, one-on-one counseling, or asking for assistance at the learning resource center where your child is receiving treatment that will help. Give yourself more confidence and strength.
Parents, other family members and friends may also go through transitions. A carer plays a very important role in supporting a child diagnosed with cancer, providing physical, emotional and practical care daily or as needed. Many caregivers are better off, especially if treatment lasts for many months or longer.
However, when treatment ends, the caregiver's role often changes. Ultimately, the care needs associated with a child's cancer diagnosis will greatly decrease or end as your child ages. Family counselors at pediatric cancer centers can help with this transition.
Children with cancer can enhance the quality of their futures by following their doctor's instructions for good health and well into adulthood, including not smoking, maintaining a healthy weight, eating Drink well, manage stress, and engage in regular physical activity. Talk to your doctor about developing a plan that's best for your child's needs.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
References: Cancer.net
MORE:
What is Chronic Lymphocytic Leukemia (CLL)? For the first time in Vietnam successfully treated T/NK cell lymphoma with immunotherapy What are lymphocytes?