This is an automatically translated article.
Posted by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital
Subarachnoid hemorrhage (SAH) is a systemic disease, and patients often have additional medical complications. Anticipating these complications leads to rapid diagnosis and treatment.
1. Cardiopulmonary complications
Cardiopulmonary dysfunction is a well-understood complication of SAH and can range from minor ECG changes to severe stress cardiomyopathy and neurogenic pulmonary edema. Rates of left ventricular failure in the first week after SAH vary from 9% to 30% and may include regional motor abnormalities that are not correlated with coronary artery size or severe left ventricular systolic dysfunction with ejection fraction. less than 30%. ECG changes may include T wave inversion and prolonged QTc interval and may be the culprit for arrhythmias such as bradycardia, atrial fibrillation, ventricular tachycardia, and ventricular fibrillation. The severity of SAH was an independent predictor of cardiopulmonary injury, suggesting that cardiopulmonary injury is neuro-mediated. An increase in troponin may be seen in up to 30% of patients, but the significance is unclear. Certain ECG changes, such as prolongation of the QTc interval, have been reported to have predictive value in mortality.
Similarities have been observed between pheochromocytoma and SAH, linking the cardiac changes observed with catecholamine "surge". Patients with SAH may experience a 3-fold increase in norepinephrine levels for 10 days or longer after disease onset, which will return to normal after this period. Myocardial necrosis, also known as contractile fascicular necrosis, is the diagnostic criterion for a catecholamine surge and can be seen in patients with pheochromocytoma and SAH. Localized central catecholamine release in the posterior hypothalamus based on postmortem pathology, found microscopic hypothalamic lesions including foci of bleeding and small infarction in patients with fibrous gangrene. muscle contraction.
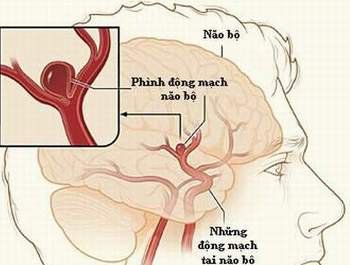
Vỡ phình động mạch sẽ trực tiếp dẫn tới tổn thương cơ tim của bệnh nhân
Clinically, the catecholamine surge in ruptured aneurysms directly leads to myocardial injury, leading to decreased myocardial contractility and increased preload for vasoconstriction, as well as increased afterload for the heart due to vasoconstriction. peripheral circuit. Consequently, ejection volume is decreased, which is not compensated by increased heart rate, leading to decreased cardiac output and neurogenic cardiogenic shock. Because of the loss of cardiac plasticity (the heart is “shocked”), the heart silhouetted on the ventricular radiographs and on the chest X-ray has the characteristic shape of a Japanese octopus basket (tako-tsubo), the reason why why this disease is also called Takotsubo cardiomyopathy. Neurogenic cardiomyopathy in SAH is associated with high mortality and poor long-term outcomes.
Pulmonary edema leading to hypoxemia is also common and may occur as a result of acute left ventricular dysfunction or independently as neurogenic pulmonary edema due to markedly increased pulmonary capillary pressure due to release of pulmonary vasculature. cold. Cardiopulmonary complications following SAH are usually transient and resolve within a few days to 2 weeks. However, during this period, the patient must be maximally supported to prevent brain damage secondary to hypoxia and decreased cerebral perfusion. In severe cases, placement of an intra-aortic balloon pump may be necessary to support the patient until the transient symptoms are resolved.
At the author's hospital - Dr Susanne Muehlschlegel, every SAH patient has ECG, echocardiogram, and chest X-ray recorded at admission. Avoid overhydration with isovolemic targets and no volume expansion. Protective mechanical ventilation of the lungs with tidal volumes below 7 cm3/kg of ideal body weight and not allowing CO2 elevation is routinely performed. If late cerebral ischemia is present and hypertension is initiated, cardiotropic agents may be used in addition to vasopressors to increase myocardial contractility. Volume expansion is limited to avoid or prevent worsening of pulmonary edema. Echocardiography was again performed 10 to 14 days after the onset of the complication to assess the recovery of Takotsubo cardiomyopathy.
2. Fever

Sốt là biến chứng nội khoa thường gặp nhất
Fever is the most common medical complication after SAH, occurring in up to 70% of patients. Fever occurs more frequently in patients with severe SAH and severe neurological status. Fever is associated with delayed cerebral ischemia and worse clinical outcomes and may be related to SIRS and chemical meningitis rather than an infectious process. While fever is usually treated with thermoregulation and isothermal therapy, there is currently no clear evidence that such treatment is beneficial. Current recommendations are to monitor body temperature and rule out or treat infectious causes. If fever is reduced with isothermal therapy, chills should be avoided and treated aggressively if present.
3. Thromboembolism and prevention
Deep vein thrombosis after SAH is common, with incidence between 2% and 20% depending on screening method. Patients with severe SAH are at higher risk, thought to be more sedentary. To prevent the life-threatening consequences of pulmonary embolism, mechanical venous thromboembolism prophylaxis should be initiated on admission with the use of a pneumatic device. At the author's hospital, pharmacological prophylaxis with subcutaneous fractionated or unfractionated heparin was usually indicated immediately after endovascular aneurysm intervention and within 24 hours of craniotomy. Thrombocytopenia due to heparin type II was seen in 6% of patients with SAH. The actual mechanism for this phenomenon is unknown. However, this syndrome should be clinically suspected immediately and diagnostic measures should be initiated and treatment initiated if the platelet count falls rapidly and the patient is already receiving fractionated or unfractionated heparin.
4. Blood sugar disorders

Hạ đường máu có thể dẫn tới rối loạn chuyển hóa não
Dysglycemia is very common after SAH because of stress and is associated with late cerebral ischemia and poor clinical outcome. However, it is still unclear if this is just an accompaniment or a cause. Hypoglycemia can lead to brain metabolic disturbances and must be avoided. In the absence of clinical trials of glycemic control in patients with SAH, current recommendations are to maintain blood glucose levels between 80 mg/dL and 200 mg/dL.
5. Hyponatremia
Hyponatremia is the most common electrolyte disturbance in SAH and may be present in up to 30% of patients. The cause is thought to be hypothalamic dysfunction, mostly due to brain salt loss because of increased concentrations of sodium-depleting diuretic peptides in the cerebral circulation. The syndrome of inappropriate secretion of antidiuretic hormone (SIADH) should always be considered but is generally uncommon in patients with SAH. Knowledge of differentiating brain salt loss from SIADH is a fundamental and crucial skill for any clinician treating patients with SAH.
It is important to note that in both brain salt loss and SIADH, the test results are similar: low serum sodium (<134 mEp/mL), low serum osmolality (<274 mmol/L). ), high urinary sodium (>20 mmol/L), and high urinary osmolality (> 100 mmol/L). The only difference is the intravascular volume status; Cerebral salt loss is a hypovolemic state, whereas patients with SIADH are isovolemic or even hypervolemic. It is extremely important to properly differentiate these two syndromes because treatment is contradictory and a misdiagnosis with incorrect treatment can lead to adverse effects for patients with SAH.
Cerebral salt loss is treated with indications for fluids and sometimes continuous intravenous infusion of hypertonic saline (1.5% to 3%) and fludrocortisone if increased diuresis and diuresis-sodium interfere with maintenance. reasonable integration. In contrast, patients with SIADH are treated with fluid restriction and sometimes increased diuresis with loop diuretics. Serum sodium as well as volume status must be closely monitored.
It is also important to test thyroid and adrenal function as well as blood sugar (>500 mg/dL may lead to pseudohyponatremia) and triglyceride levels to target other causes of hyponatremia. Pseudohyponatremia (not due to true hyponatremia but to laboratory interference from hypertriglyceridemia) should be considered in patients receiving propofol.
6. Anemia

Thiếu máu thường xảy ra với bệnh nhân SAH
Most patients with SAH will develop anemia during their hospital stay, which is thought to be due to extensive blood draw, blood loss from other causes, or systemic inflammation. Anemia and hemoglobin levels below 9 g/dL are associated with late cerebral ischemia and poor clinical outcomes; however, the optimal hemoglobin concentration target and transfusion threshold are unknown. A recent small randomized controlled trial comparing the safety and efficacy of transfusion for higher hemoglobin concentrations (target hemoglobin concentration of at least 10 g/dL or 11.5 g/dL) in patients with SAH demonstrated the safety of transfusion to those hemoglobin concentrations, but no difference in late ischemic stroke and short-term functional outcome (14 days).
7. Prognosis after subarachnoid hemorrhage
While existing clinical scores such as WFNSS and Hunt and Hess can be useful in differentiating high-risk from low-risk patients, they are not different from any other prognostic scale, they were designed designed for the population rather than for a specific patient.
Outcomes are also influenced by many other factors, which are not generally included in prognostic scales, such as cost and patient choice, comorbidities, social network, tolerance, and recovery time. Unless the patient has bilateral mydriasis and a head CT or DSA is unsatisfactory for cerebral perfusion and survival, all efforts should be made at the outset to save even very severe SAH patients with Measures to treat hydrocephalus and increase ICP, followed by aneurysm occlusion. Appropriate neuro-active therapy should be provided for at least the first 2 weeks or so, at a time when, after determining the patient's prior wishes and family preferences, Further goals of care may need to be discussed. The FRESH Functional Recovery Expectation Scale (FRESH) is a newly published prognostic score for cognitive outcomes and expected quality of life 12 months after SAH, and requires similar caution with this scale as with any other prognostic scale. This scale has good discrimination and measurement, is proven, and can be calculated at the bedside using a free smartphone app.
Conclusion
SAH is a life-threatening hemorrhagic stroke and a neurological emergency with a high risk of disability and death. This female-predominant disease requires a two-phase approach: (1) rapid and accurate diagnosis of SAH, referral to an appropriate bulk center, and identification and occlusion of the aneurysm, and (2) Observation, prevention, or referral of neurologic and medical complications in a neuro-intensive care unit with skillful neurosurgery in line with established guidelines. Major neurological complications include hydrocephalus, seizures, cerebral edema, and delayed cerebral ischemia. Common medical complications, including cardiopulmonary complications, neuroendocrine disorders, and fever, require competent management.
Source:
Susanne Muehlschlegel, MD, MPH, FNCS, FCCM “Subarachnoid hemorrhage” CONTINUUM (MINNEAP MINN) 2018;24(6, NEUROCRITICAL CARE): 1623–1657