This is an automatically translated article.
Posted by Doctor Le Van Binh - Intensive Care Unit - Vinmec Times City International HospitalRespiratory failure is a very common condition that can be life-threatening in infants. Currently, there are a number of respiratory failure diseases in infants that need to be detected early and treated promptly to prevent dangerous complications for the child.
1. Diaphragm hernia
The incidence of diaphragmatic hernia in children accounts for about 1/2000-3000 cases. Often children will have a hernia on the left side, the abdominal organs take the place of the lung in the thoracic cavity, causing pulmonary hypoplasia. Currently, diaphragmatic hernia can be diagnosed prenatally by fetal ultrasound.
Infants with diaphragmatic hernia will have respiratory failure soon after birth, with manifestations of cyanosis and severe hypoxia. On examination, the right apex of the heart beats, the chest is inflated, the left alveolar murmur is not seen, and the abdomen is flat.
X-ray is valuable in diagnosing diaphragmatic hernia in children. The results will show the bowel in the thoracic cavity, mediastinum is pushed to the opposite side (usually right), atelectasis of the healthy side. If a contrast tube is placed into the stomach, the position of the stomach will be determined on the film.
Management of diaphragmatic hernia in infants:
Place the child in a 45o position, leaning to the side of the patient; Insert a nasogastric tube to deflate the stomach; No respiratory aid through the mask; Intubation, mechanical ventilation; Intravenous infusion of glucose, to ensure acid-base balance, to keep the child's temperature stable; Foreign transfer, emergency surgery. The mortality rate for children with diaphragmatic hernia is about 50-60%.
2. Atrophy of the esophagus causes respiratory failure
Neonatal esophageal atrophy accounts for 1/3000-4000 live cases. Of which, 1/3 are premature babies, 90% have esophageal-tracheal fistulas.
Neonatal esophageal atrophy is divided into 4 types:
Type 1: Simple esophageal atrophy (7.5-10%); Type 2: Esophageal atrophy + esophageal-tracheal fistula in the uppermost sac (1-2%); Type 3: Esophageal atrophy + esophago-tracheal fistula in the lower sacrum (86%); Type 4: Esophageal atrophy + esophago-tracheal fistula in the upper and lower sacrum (1-5%); Atrophy of the esophagus can be diagnosed before birth by fetal ultrasound, after 24 weeks. After birth, the baby will have respiratory failure, increased sputum secretion, flat abdomen. When the nasogastric tube was inserted, the tube was extruded back.
Standing film, with the tube in place, 10ml of air through the tube (or 0.5ml of water-soluble contrast) allows the location of the uppermost esophageal pouch to be determined. In type 1+2: There is no air under the diaphragm, the abdomen is white. in type 3+4: There is a lot of air in the abdomen.
50% of children with esophageal atresia have other malformations such as: spine, anus, heart, kidneys, limbs.
Children with esophageal atrophy due to chromosomal abnormalities account for 8-27%, most commonly 3 chromosomes 18 and 21.
Treatment of children with esophageal atrophy causing respiratory failure:
Position 45o, leaning to one side. side to avoid reflux; Suction sputum continuously. Atropine 0.02 mg/kg can be used before transferring to the surgical department to reduce sputum production; Fasting, intravenous infusion; No mask-assisted respiration because airflow through the fistula widens the esophageal-tracheal fistula; Intubation, mechanical ventilation can also cause gastric rupture in case of large fistula. In case it is necessary to intubate deeper than the position of the fistula; Emergency surgical transfer The mortality rate for children with esophageal atresia accounts for about 10%.

3. Pneumothorax
Pneumothorax occurs when an elderly child has respiratory failure, aspirates meconium amniotic fluid, is receiving respiratory aid through a mask, or breathes oxygen through a high-pressure catheter.
Through examination, the chest will be unbalanced, the alveolar murmur is lost on one side, the apex of the heart is deviated to the healthy side, and the abdomen is distended. A chest X-ray is required for a definitive diagnosis.
Management:
Aspiration, air drainage: Can use Valium 0.3 mg/kg intravenously or Katalar 2 mg/kg intravenously before drainage so that the child does not have pain during puncture; Respiratory aid if needed.
4. Transient respiratory distress syndrome (pulmonary resorption)
Normally after birth, there will be no fluid in the alveoli of the baby. For some reason, such as an indication for an elective cesarean section before labor, the baby's birth too quickly, the use of β-blockers in the mother, etc., there will still be fluid in the alveolar lumen that obstructs ventilation and lead to respiratory failure in children.
Clinical manifestations of transient respiratory distress syndrome: The child has very rapid breathing (usually over 100 beats/min), subtle chest retraction and moderate respiratory distress.
Chest X-ray shows interstitial syndrome, clear interlobular groove, possibly pleural effusion.
Treatment: Give the child oxygen through a tube, respiratory aid if needed. Good prognosis.
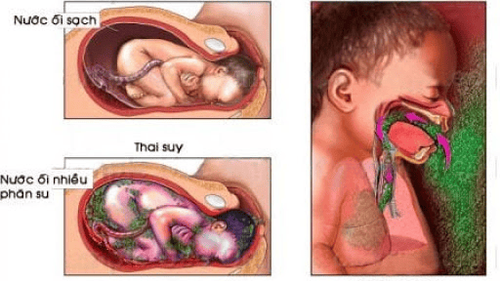
5. Inhalation of amniotic fluid meconium
Meconium aspiration syndrome often occurs in pregnant women with acute fetal distress, which is a state of hypoxia and acidosis, leading to the excretion of meconium into the amniotic fluid. Along with the inhalation movement will cause feces to enter the child's lungs.
Meconium aspiration syndrome often occurs in full-term infants who are too large or have the placenta wrapped around their neck.
In case the newborn has respiratory failure and meconium amniotic fluid, it is necessary to clear the nasopharynx and intubate immediately, and at the same time aspirate fluid through the endotracheal tube to avoid spreading the meconium amniotic fluid into the small bronchi. cause pulmonary edema.
If the child's condition improves, leave the endotracheal tube in place for 24 - 48 hours for the purpose of frequent endotracheal aspiration. Limit mechanical ventilation.
In case the chest X-ray shows scattered opacities throughout the 2 lung fields, collapsed lung segments, it is necessary to look for meconium in the urine to confirm the diagnosis.
In cases of very severe respiratory failure, it is necessary to put the child on a ventilator, to limit the metabolic acidosis caused by the lack of cellular oxygen, which aggravates the respiratory failure.
Treatment: In addition to ensuring oxygen demand, acid-base balance, and circulating volume with macromolecular solutions, we can use talazoline (non-specific α-inhibitor) to reduce vasospasm. Pulmonary system at a dose of 1-2 mg/kg infused by central venous catheter into superior vena cava or right atrium over 10 minutes (close arterial blood pressure monitoring) then maintained at 1-2 mg/kg/ hours, reduce the dose gradually. Currently, the use of NO does not cause hypotension complications.
Mortality rate in children who aspirate meconium amniotic fluid is still high (about 50%). Leaving severe neurological and renal sequelae in survivors.
6. Inner membrane disease
Inner membrane disease accounts for 1% of all newborns, 10% of premature babies, 50% of babies born less than 30 weeks. Currently, the use of glucosteroids for mothers with threatened preterm labor has significantly reduced the morbidity and severity of endocarditis in infants.
Clinical and subclinical signs of endocardial disease:
Typically right after birth or within the first 6 hours of life, the baby appears respiratory distress, rapid breathing over 60 times a minute, respiratory muscle contractions clear breathing, nasal flaps and bulges, groaning sound during exhalation, weak alveolar murmurs, cyanosis. Progressive worsening within 24 hours. During this time, it can be dangerous to the life of the child if there is no respiratory aid. After 2-3 days can improve slowly. Severe disorders of blood gases: PaO2 decreased up to 50 mmHg, PaCO2 increased above 70 mmHg, pH decreased. Chest X-ray helps to confirm the diagnosis of carrier disease: Small opacities throughout the 2 lung fields and the tracheobronchial system are too bright on the film. Based on chest radiograph, endocardial disease is divided into 4 degrees: +Grade 1: small opacities throughout the two lung fields;
+Grade 2: Grade 1 + clearly see the bronchial system outside the heart shadow;
+Grade 3: Grade 2 + clearly delineates the heart's boundaries;
+ Grade 4: white lungs.
Treatment:
Symptomatic treatment:
Minimize unnecessary touches to children with respiratory failure. Taking samples for testing and taking X-rays must also be gentle. Children with little discharge should be endotracheal suctioned every 6 hours; Monitor arterial blood pressure, keep the child's temperature stable; Measure blood gas to adjust the ventilator and oxygen concentration in accordance with the child's requirements (make sure PaO2 40®-70 mmHg in capillary blood); Nasal CPAP with 5-7 cm of water when oxygen demand is above 50%. Using CPAP early will save surfactant, reduce lung complications and better prognosis; Mechanical ventilation when respiratory failure worsens, when oxygen demand is above 60%, or PCO2 is above 50-60 mmHg with PEEP of 4 cm of water; Antibiotics: In case of suspected bacterial infection, use β-lactamin + gentamycine. Stop antibiotics after 5 days if there are no clinical and laboratory signs of infection; Protein infusion 1g/kg/24 hours because surfactant synthesis consumes a large amount of protein; Ensure blood sugar for children with glucose solution; Pay attention to water intake to avoid the existence of ductus arteriosus and avoid renal failure. 70 ml/kg/24 hours is reasonable; Ensure acid-alkaline balance; Pay attention to early detection of ductus arteriosus for prompt treatment. Using surfactant: There are two main types: natural surfactant and synthetic surfactant. Surfactant is injected into the lungs through the endotracheal tube
Animal surfactant: Originated from bovine (Survanta: 100mg/kg, Alveofact); Calf origin (Infasurf, BLES); Originated from pigs (Curosurf: 100-200 mg/kg). Synthetic surfactant: Alec (Pum actant); Surfexo; Newfactant... Prevention:
Prevention of pregnancy in infants by administering Betamethasone (12mg IM x 2 24 hours apart) to the mother in case of threatened preterm birth under 34 weeks of age and 24-72 hours before birth to help lung cells 2 produce surfactant. The drug is effective from 24 weeks, helping to reduce the frequency and severity of respiratory failure. Lung maturity was also assessed by the ratio of Lecithin/Sphingomyelin in the amniotic fluid. If this ratio is < 2, the possibility of postpartum respiratory failure is very high. Pregnant women need to use drugs to reduce uterine contractions and antibiotics to prevent infection in case of need.

7 Lungs are too young
Common in premature infants < 1500g, especially under 1000g. At this time, the child's lung organization is too young and does not take on the task of gas exchange.
In the fetal stage, alveolar cells are thick, cylindrical, capillary walls are thick, cells are also cylindrical; The interstitial organization between alveoli and capillaries is wide, containing a lot of glycogen. Therefore, there is almost no gas exchange between the alveoli and capillaries. From the 28th week, alveolar cells and capillaries gradually flatten, alveolar and capillary walls thin, the distance between alveoli and capillaries narrows, allowing gas exchange to occur easily.
If the baby is born before that time, the gas exchange between the blood and the alveoli is not good, the child has respiratory failure, dies in the context of pulmonary hemorrhage or atelectasis.
8. Lung infections
Common because the child's immune system is not working well.
Early infection (mother-infant infection) is often in the context of systemic infection, sepsis.
Symptoms of respiratory failure may be masked by systemic symptoms such as purple veins, shock, groaning, and decreased muscle tone.
Atypical chest radiograph: Uneven opacities scattered in 2 lung fields. May be misdiagnosed as endocarditis in premature infants.
Lung infection due to mother-infant infection:
C can be caused by blood sugar or by inhalation of contaminated amniotic fluid at birth; Bacteria are detected by blood cultures, in gastric juices, in peripheral specimens or sometimes in cerebrospinal fluid; Some common bacteria are Streptocoque B, E. Coli ; Treatment: β-lactamine + intravenous gentamycin. If treated late, it will cause septic shock or irreversible severe hypoxia, especially for Streptococcus B. Hospital-acquired lung infections:
Usually occurs in premature infants in the emergency room, requiring intubation long-term management - mechanical ventilation; Bacterial strains that enter the lower respiratory tract of children are due to endotracheal aspiration, they will reside there more than 1 week after intubation. Find pathogenic bacteria by culture of bronchoalveolar lavage fluid. Common bacteria are Staphylococcus aureus or epidermidis, Gram (-) bacilli such as Enterobacteriesn, Pseudomonas. Treatment: Staphylococcus aureus: Vancomycine + Aminozide; Fosfomycine + Cefotaxime; Gram (-) bacilli: Use 3rd generation Cephalosporin C + Aminoside. In preterm infants with intubation, increased need for 02, chest radiograph showing alveolar lesions - interstitial tissue must set the differential diagnosis between pneumonia, pulmonary edema due to ductus arteriosus and dysplasia. lung-bronchi. Viral lung infections:
May be seen in premature babies because of contact with healthy carriers; Common viruses are: Respiratoire syncitic (VRS), Myxovirus parainfluenzae. Virus detection in nasopharyngeal fluid by immunofluorescence or culture. Superinfection is usually caused by Haemophilus influenzae, Pneumocoque. Infection with VRS can be mild but can also cause severe respiratory failure, especially in individuals with pulmonary-bronchial dysplasia, congenital heart disease. Treatment with nebulized Ribavirine, which is specific for VRS. As soon as the child shows symptoms of severe respiratory failure, parents need to take the child to a reputable hospital to be consulted by a specialist for monitoring and treatment. Currently, the Pediatrics Department at Vinmec International General Hospital is trusted by many parents to examine the diseases that infants and young children are susceptible to. Vinmec brings satisfaction to customers and is highly appreciated by industry experts by:
Gathering a team of leading pediatricians: Including leading experts with high professional qualifications ( professor, associate professor, doctorate, master), experienced, worked at major hospitals such as Bach Mai, 108.. The doctors are well-trained, professional, have a heart - a vision. Understanding young psychology. In addition to domestic pediatric specialists, the Department of Pediatrics also has the participation of foreign experts (Japan, Singapore, Australia, USA) who are always pioneers in applying the latest and most effective treatment regimens. . Comprehensive services: In the field of Pediatrics, Vinmec provides a series of continuous medical examination and treatment services from Newborn to Pediatric and Vaccine,... according to international standards to help parents take care of their baby's health from birth to childhood. upon reaching adulthood. Advanced techniques: Vinmec has successfully deployed many specialized techniques to make the treatment of difficult diseases in Pediatrics more effective: neurosurgery - skull surgery, hematopoietic stem cell transplantation in cancer treatment. Professional care: In addition to understanding children's psychology, Vinmec also pays special attention to the children's play space, helping them to play comfortably and get used to the hospital's environment, cooperate in treatment, improve the efficiency of medical treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.