This is an automatically translated article.
Skin grafting is surgery that involves removing skin from one area of the body and moving or transplanting it to another area of the body that needs them. This surgery can be done when a part of your body has lost its protective skin due to a burn, injury, or disease.
1. What is a skin graft?
Skin grafting is surgery that involves removing skin from one area of the body and moving or transplanting it to another area of the body that needs them. This surgery can be done when a part of your body has lost its protective layer of skin due to a burn, injury, or disease.
Skin grafts are done in the hospital. Skin grafts are mostly done under general anesthesia, which means you'll be asleep during the procedure and won't feel any pain.
2. Why is skin grafting done?
Skin graft is implanted on a lost skin area of the body. Common reasons for skin grafts include:
Skin infections. Deep burns. Large open wound. Bed sores or other sores on the skin that have not healed completely. Skin cancer surgery. Skin graft to treat scars.

Ghép da được cấy ghép trên một vùng da bị mất của cơ thể.
3. Types of skin grafts
There are two basic types of skin grafts, namely: Thin skin graft and full thickness graft.
3.1. Separate thickness grafting This is an individual layer of skin grafting that involves removing the top layer of skin (epidermis) as well as part of a deeper layer of skin, called the dermis. dermis. These layers are taken from the donor site, which is an area of healthy skin. Thin-thickness skin grafts are usually taken from the front side, called a face transplant, or the outside of the thighs, abdomen, buttocks, or back can be removed.
Pieces will be subdivided in thickness to cover a large area. These puzzle pieces are fragile in nature and often have a shiny or smooth appearance. They may also be lighter in color than the adjacent skin. Detached thickness grafts don't grow as easily as non-grafted skin, so children who receive them may need additional grafts as they grow.
3.2. Full-thickness grafting Full-thickness grafting is the removal of all of the epidermis and dermis from the donor site. The abdomen, groin, forearm, or the area above the collarbone (clavicle) are the places that are usually taken. They tend to be smaller, as the donor site is usually pulled together and closed into a straight line with sutures or staples.
Full-thickness grafts are often used for minor injuries in visible parts of the body, such as the face. Unlike low-thickness grafts, full-thickness grafts blend well with the skin around them and often provide better cosmetic results.
4. How to prepare for skin grafting
Your doctor will probably schedule your skin graft several weeks in advance, so you'll have time to prepare for the surgery. Tell your doctor if you are taking any prescription or over-the-counter medications. Some medications, such as aspirin, can reduce blood clot formation. Your doctor will direct you to change the dose or stop taking these medications before surgery. Also, smoking or tobacco preparations will decrease your skin graft's ability to heal, so your doctor will likely ask you to stop smoking before surgery.
Your doctor also tells you not to eat or drink anything after midnight on the day of the procedure. This will keep you from vomiting and choking during surgery if the anesthetic makes you nauseous.
You should also have a family member or friend to drive you home after surgery. General anesthesia can make you drowsy after the procedure, so you should have someone else drive until the effects of the anesthesia wear off.
You should also have someone stay with you for the first few days after surgery. You may need assistance to perform certain tasks and get around the house.
5. Skin grafting process
The surgeon will begin by removing the skin from the donor site. If you are having a thin-thickness skin graft, the skin will be removed from an area of the body that is normally hidden by clothing, such as the hip or the outside of the thigh. If you are receiving a full-thickness transplant, the abdomen, groin, forearm, or the area above the collarbone (clavicle) is the preferred organ donation site.
After the skin is removed from the donor site, the surgeon will carefully place it over the implant area and secure it with surgical tape, staples, or sutures. If it is a piece with a separate thickness, it can be “mesh”. The graft will have many holes punched by the doctor to stretch the skin out, so they will take less skin from your donation site. This also allows fluid to drain from under the graft. Fluid accumulation under the graft can cause it to fail. In the long run, mesh grafting can give the graft a “fish net” appearance.
The doctor also covers the donor skin with a bandage that will cover the wound without sticking to it.
Trong vòng 36 giờ, mảnh ghép da sẽ bắt đầu phát triển các tân mạch máu
6. Care after skin grafting
Medical staff will monitor vital signs after surgery as well as administer medication to control pain. If you've had a thin-thickness skin graft, your doctor will likely keep you in the hospital for a few days to make sure that the graft and the donor site are healing.
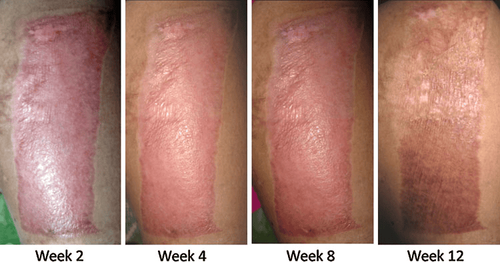
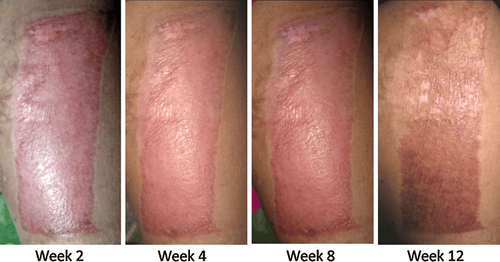
Within 36 hours, the graft will begin to grow new blood vessels and connect to the surrounding skin. If these blood vessels do not begin to form immediately after surgery, this indicates that your body is rejecting the graft.
Your doctor may tell you that the graft is “not done”. This can be for a number of reasons including infection, hematoma or fluid under the graft as well as excessive movement of the graft over the wound. This can also happen if you smoke or have poor blood flow to the transplanted area. You may have to have surgery again with a new graft if the first graft fails.
When you leave the hospital, you will be prescribed pain medication by your doctor. They will also teach you how to take care of the transplant site and the donor site so they don't get infected.
Donor sites heal within one to two weeks, but grafts take longer. For at least three to four weeks after surgery, you'll need to avoid any activity that could stretch or injure the graft site. Your doctor will tell you when it is safe to resume your normal activities.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: healthline.com, nhs.uk