This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Compelling evidence supports an important role for the receptor for the activation of the advanced glycation end product axis (advanced glycation end product receptor) in many clinical entities. Since the onset of the 2019 coronavirus pandemic, there has been growing concern about the risk and management of acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in inflammatory digestive disorders. , such as inflammatory bowel disease (IBD).
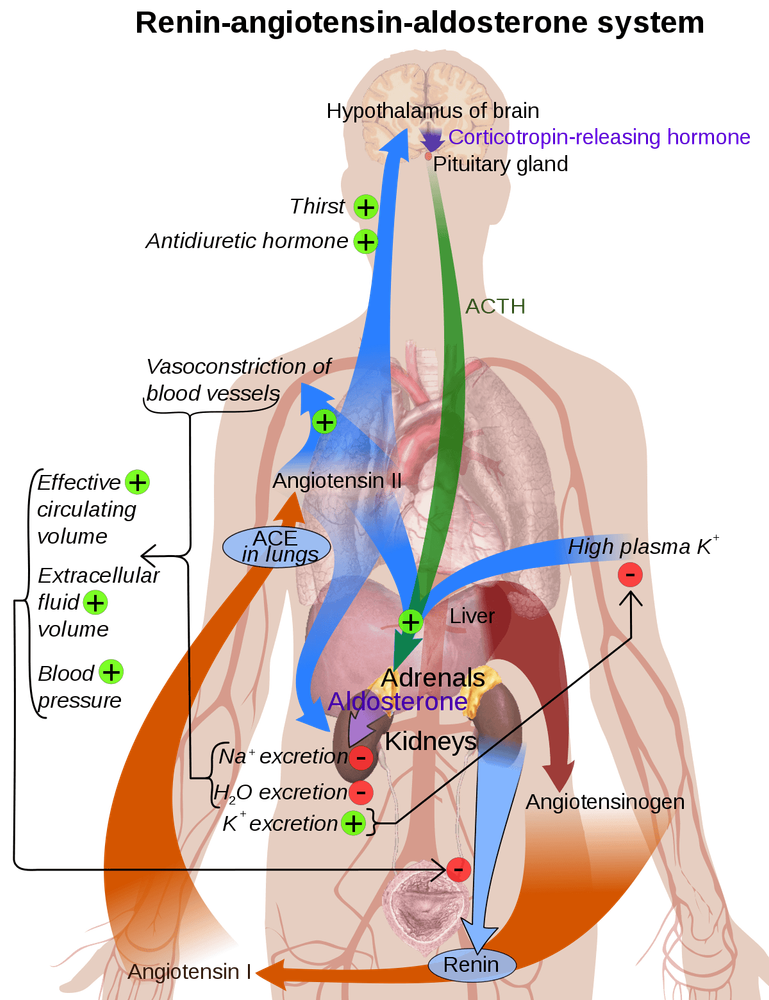
1. What is the renin-angiotensin system?
The renin-angiotensin system (renin-angiotensin system) is a hormonal system regulated by two complementary pathways that mediate opposing effects on inflammation, fibrosis, and cell proliferation cell. Thus, the balance of both pathways determines the proinflammatory or anti-inflammatory status between several systems such as the cardiovascular, renal, and respiratory systems.
The classical pathway is mediated by ACE, angiotensin II (Ang II) and its Ang II receptor type 1 (AT1R), triggering activation of pro-inflammatory signaling such as oxidative and nitrosative stress, induction cytokines and cell adhesion molecules, as well as the activation of transcription factors such as NF-κB. In contrast, the alternative pathway is mainly mediated by ACE2, Ang (1-7) and its Mas receptor (MasR), which induce the opposite effects of AT1R activation, which is a regulator of AT1R. Anti-inflammatory and anti-fibrotic effects of ACE. / Ang II / AT1R. ACE and ACE2 are abundantly expressed in several tissues such as the lungs, kidneys, and blood vessels. However, the brush border of the ileum and colon was among the tissues with the highest expression of both enzymes. Both enzymes are able to cleave angiotensin, producing different by-products and regulating the balance between both pathways of the renin-angiotensin system.
2. Balancing the renin-angiotensin system in inflammatory bowel disease
Recent studies show elevated expression of key components of both the renin-angiotensin system pathways across the ileum and colon. In this sense, the gut may be an organ that is particularly sensitive to imbalances of the renin-angiotensin system pathways. Thus, dysregulation of these components may have potential inflammatory and fibrotic effects in IBD patients. Notably, several studies have revealed that gut expression of ACE2 is inversely correlated with fibrosis in patients with inflammatory bowel disease.
In addition, Ang (1-7) improves colonic fibroblast collagen secretion through MasR. Furthermore, angiotensin receptor blockers and ACE inhibitors have been reported to reduce proinflammatory cytokines, ameliorate colitis, and are associated with lower rates of complications, surgery, and hospital admissions in this patient. inflammatory bowel disease patients.
3. Bioavailability of ACE2
Normally, ACE2 degrades Ang II into Ang 1-7 peptides and thus avoids activation of the proinflammatory pathways of the renin-angiotensin system. However, SARS-CoV-2 is able to hijack ACE2 and use it to enter host cells. Notably, high bioavailability of soluble ACE2 has been reported in patients with inflammatory bowel disease, mainly due to the increased levels of ADAM17 observed in these patients. Therefore, it is possible to act as a decoy receptor for SARS-CoV-2 and avoid counter-enzyme attack.
This is particularly important considering that a novel ligand-independent mechanism for advanced glycation end-product receptor metabolism was recently reported to occur after AT1R activation by Ang-II . Thus, leading to NF-B-dependent expression of inflammatory mediators
4. Advanced glycation end-product receptor axis activity and renin-angiotensin system balance in SARS-COV-2-infected inflammatory bowel disease
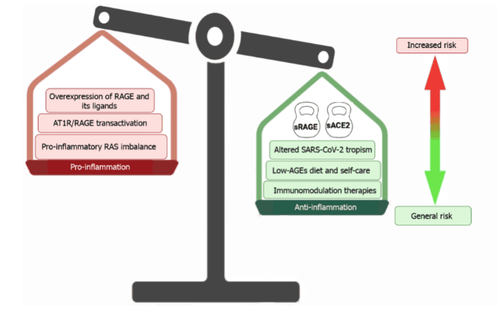
Contrary to what would be expected, in view of the pathophysiology of inflammatory bowel disease, there is currently no evidence of an increased risk of worse clinical outcomes in IBD patients in the context of the COVID-19 epidemic- 19 . The role of the advanced glycation end product receptor axis in the pathophysiology of inflammatory bowel disease has been suggested by various reports. Colonic expression of advanced glycation end product receptor and some advanced glycation end product receptor ligands, such as HMGB1 and some members of the S100 protein family, was significantly higher in patients inflammatory bowel disease. In addition, this receptor is also implicated as a major contributor to the dysregulated and misdirected COVID-19 inflammatory response.
However, a counterweight must be added to this scenario: the soluble advanced glycation end product receptor. This molecule is generated by alternative splicing or by ectodomain cleavage of the membrane-anchored advanced glycation end product receptor by the action of both MMP-9 and ADAM17, which are highly expressed in patients with inflammatory bowel disease. . Therefore, the high bioavailability of the soluble advanced glycation end product receptor may reduce advanced glycation end product receptor activation. Despite the abundance of both receptors and ligands in the inflamed intestinal mucosa of patients with inflammatory bowel disease.
5. Inflammatory bowel disease of patients with inflammatory bowel disease may be favorable conditions for the entry of SARS-CoV-2
On the other hand, the high expression of ACE2 in the gastrointestinal tract, especially in patients with inflammatory bowel disease makes this tissue a particularly susceptible nutritional niche for SARS-CoV-2 infection. Furthermore, depletion of ACE2 by entry of SARS-CoV-2 may subsequently induce a strong renin-angiotensin system imbalance in favor of the inflammatory ACE/Ang II/AT1R pathway. These observations suggest that the inflamed gut of IBD patients presents an optimal gateway for SARS-CoV-2 entry, leading to poor clinical outcomes in IBD patients who develop COVID. -19.
However, this hypothetical scenario also has an important counterpoint, the soluble form of ACE2, which is also increased in patients with inflammatory bowel disease due to the shedding of membrane-bound ACE2 by ADAM17. This is particularly important considering the described non-cognate metabolism mechanism for the advanced glycation end product receptor because activation of AT1R by Ang II is prevented by the maintenance of ACE2 depletion. related to the membrane in its soluble form.
6. Role of systemic immunosuppressive drug use on increased risk of COVID-19 in patients with inflammatory bowel disease
There is increasing evidence that in patients with IBD, systemic immunosuppressive use is not associated with an increased risk of COVID-19 in IBD patients. Furthermore, we must also keep in mind that the main goal of drug treatments in inflammatory bowel disease is to reduce the level of inflammation. In this sense, in addition to interfering with signaling pathways, many drugs used in current treatments also reduce advanced glycation end-product receptor expression and the bioavailability of a advanced glycation end-product receptor ligands, especially the HMGB1 and S100 protein family members of HMGB1 and S100. Indeed, some authors have commented on a possible protective role of inflammatory bowel disease therapy against SARS-CoV-2 infection, particularly through interference with the cytokine activity observed during clinical course of COVID-19.
In addition, IBD patients have high self-care standards and follow a diet that helps them maintain good nutrition and keep their illness under control. Some of these diets are associated with low-age diets, which may contribute to the reduction of proinflammatory intestinal tissue mediated by advanced glycation end-product receptor activation.
7. Inflammatory mechanisms are activated in patients with SARS-CoV-2
Among them, receptor overexpression of advanced glycation end products (advanced glycation end product receptor) and an abundance of its ligands can induce sustained activation of the axis, may also be promoted by a non-cognate mechanism due to an imbalance in inflammatory rat sarcoma.
These factors appear to be important contributors to the worsening of inflammatory bowel disease (inflammatory bowel disease) in patients with coronavirus disease 2019. However, other factors may reduce these contributions. These inflammatory contributors, such as the high bioavailability of soluble forms of both advanced glycation end-product receptors and the enzyme-converting angiotensin 2. Soluble angiotensin 2 converting enzyme may even interfere with invasion entry of coronavirus 2 causes severe acute respiratory syndrome into epithelial cells.
In addition, most if not all patients with IBD are on drug therapy to control inflammation. Inflammatory bowel disease patients need special attention to their diet and the consumption of advanced glycation end products in the diet is also limited.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Rojas A, Schneider I, Lindner C, González I, Morales MA. Receptor for advanced glycation end-products axis and coronavirus disease 2019 in inflammatory bowel diseases: A dangerous liaison? World J Gastroenterol 2021; 27(19): 2270-2280 [DOI: 10.3748/wjg.v27.i19.2270]