This is an automatically translated article.
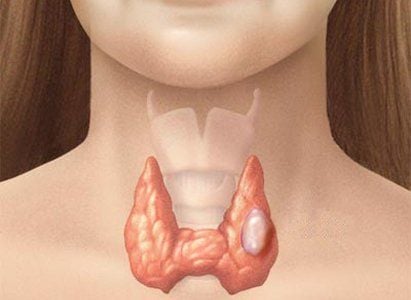
The thyroid gland produces hormones that regulate heart rate, blood pressure, body temperature, and weight. Thyroid cancer occurs in the cells of the thyroid gland located at the bottom of the neck. In the United States, thyroid cancer ranks fifth of all cancers in terms of prevalence. So, what are the risk factors for thyroid cancer?1. Unmodifiable thyroid cancer risk
Gender and age
For reasons that are not clear, the incidence of thyroid cancer in women (like most thyroid diseases) is about 3 times higher than in men.
Thyroid cancer can occur at any age, but the risk peaks earlier for women (usually in their 40s or 50s when diagnosed) than for men (usually when diagnosed). diagnosed at age 60 or 70).
Genetic diseases
Several genetic conditions and family history are associated with different types of thyroid cancer. However, most people who develop thyroid cancer do not have an inherited condition or a family history of the condition.
Medullary thyroid cancer: About 2 out of 10 medullary carcinomas (MTCs) are caused by abnormal genes. These cases are called medullary thyroid carcinoma (FMTC). FMTC may occur alone or it may be detected along with other tumors. The combination of FMTC and tumors of other endocrine glands is called multiple endocrine neoplasia type 2 (MEN2). There are two forms of this type, MEN 2a and MEN 2b, both caused by mutations in a gene called RET. In MEN 2a, MTC occurs with adrenal myeloma (adrenaline-producing tumor) and with parathyroid tumor. In MEN 2b, MTC is associated with adrenal myeloma and benign growths of nerve tissue on the tongue and elsewhere called neuromas. This type is much less common than MEN 2a. In these inherited types of MTC, the cancer usually develops during childhood or early adulthood and can spread early. If MEN 2a, MEN 2b, or FMTC runs in your family, you may be at very high risk for MTC. Therefore, you should consult your doctor about regular blood tests or ultrasound exams to look for symptoms and genetic testing.

Ung thư tuyến giáp có thể xảy ra do di truyền
Other thyroid cancer: People with certain genetic diseases have an increased risk of more common forms of thyroid cancer. A higher rate of thyroid cancer occurs in people with an uncommon genetic condition such as:
Familial adenomatous polyposis (FAP) : People with this syndrome have signs of developing multiple polyps colon and have a very high risk of colon cancer. They also have an increased risk of several other cancers, including papillary thyroid cancer. Gardner syndrome is a type of FAP in which the patient also has several benign tumors. Both Gardner syndrome and FAP are caused by defects in the APC gene. Cowden's disease: People with this syndrome are at increased risk for thyroid problems and certain benign growths. They are also at risk for cancers of the thyroid, uterus, breast, as well as several other organs. Thyroid cancer tends to be papillary or follicular type. This syndrome is usually caused by a defect in the PTEN gene.

Hội chứng Cowde được gọi là hội chứng đa u lành tính xảy ra do khiếm khuyết trong gen PTEN.
Carney complex disease (type I): People with this syndrome can develop some benign tumors and have hormone problems. They are also at increased risk for papillary and follicular thyroid cancer. This syndrome is caused by a defect in the PRKAR1A gene. Familial nonmedullary thyroid carcinoma: This type of thyroid cancer occurs more often in some families and is often discovered at a very young age. Currently, scientists are suspecting that mutations in genes on chromosome 19 and chromosome 1 cause this type of cancer. Family history
Having an immediate relative (parent, brother, sister, or child) with thyroid cancer, even without a family history of the syndrome, increases the risk of thyroid cancer your. The genetic basis for these cancers is not entirely clear.
2. Risk factors that can be changed
Radiation
Radiation exposure is a proven risk factor for thyroid cancer. Such emission sources include certain medical treatments and fallout from power plant or nuclear weapon failures.
Having radiation therapy to the head or neck going on in a child is a risk factor for thyroid cancer later in life. The risk depends on the radiation level and the age of the child. In general, the risk increases with larger doses and the younger the child is on treatment.
Before the 1960s, children were sometimes treated with low doses of radiation for conditions that are no longer used, such as acne, scalp fungal infections, or enlarged tonsils or adenoids. Years later, people receiving this treatment were found to be at high risk for thyroid cancer. Radiation therapy in childhood for certain cancers such as lymphoma, Wilms tumor, and neuroblastoma also increases the risk. Thyroid cancer that develops after radiation therapy is no more serious than other thyroid cancers.

Phơi nhiễm phóng xạ là một yếu tố nguy cơ có thể được thay đổi
Imaging tests such as X-rays and CT scans also expose children to radiation but at much lower doses, so it is not clear that these imaging techniques may increase the risk of cancer thyroid cancer (or other cancers). If there is an increased risk it is likely to be very small, but to be safe, children should not have these tests unless they are absolutely necessary. When necessary, the child should only be taken using the lowest dose of radiation that will still provide a clear image.
Several studies have shown an increased risk of thyroid cancer in children due to fallout from nuclear weapons or power plant failures. For example, thyroid cancer is several times more common in children living near Chernobyl, where the 1986 nuclear plant accident exposed millions of people to radiation. Adults who participated in the cleanup after the accident and those who lived near the factory also had higher rates of thyroid cancer than elsewhere. Children with more iodine in their diet seem to have a lower risk.
Exposure to radiation as an adult has a low risk of thyroid cancer.
Overweight or obese
According to the International Agency for Research on Cancer (IARC), people who are overweight or obese have a higher risk of developing thyroid cancer than people of normal weight. The risk increases as body mass index (BMI) increases.
Dietary Iodine
Thyroid cancer is common in areas of the world where people eat very little iodine. On the other hand, a diet high in iodine may increase the risk of papillary thyroid cancer. In the United States, most people get enough iodine in their diets because it is added to table salt and other foods.

Những người béo phì tăng nguy cơ mắc bệnh ung thư tuyến giáp
Early detection of early signs of cancer through diagnosis imaging, endoscopy and ultrasound. The operation is simple, careful and accurate. A team of well-trained specialists, especially in oncology, are capable of handling cancer cases. With facilities, advanced and modern medical equipment and a team of doctors with deep expertise and experience. At Vinmec, the examination process becomes quick with accurate results, saving costs and time for patients.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
References: cancer.org, cancer.net, mayoclinic.org