This is an automatically translated article.
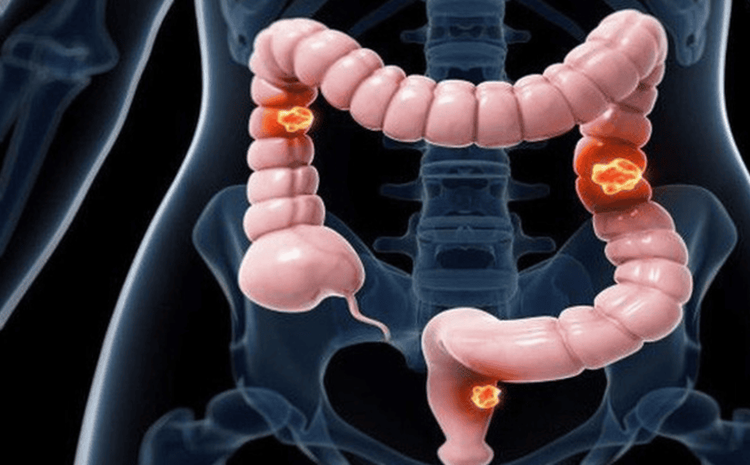
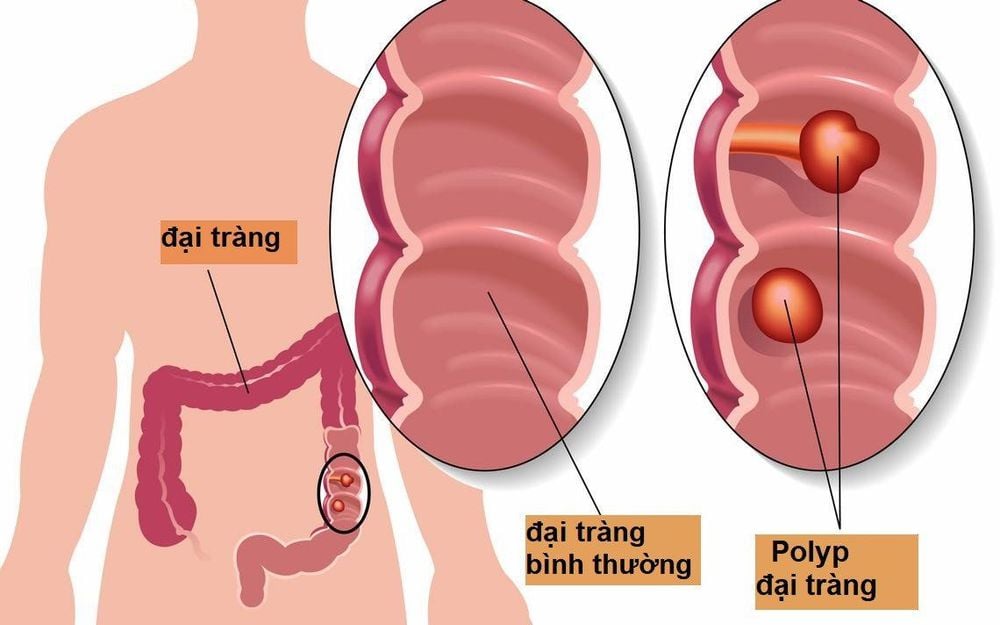
Colon cancer usually occurs in older adults, although it can occur at any age. It usually begins as small, benign masses of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancer. So what is the risk of colon cancer that increases the chance of getting this type of cancer?1. Modifiable colorectal cancer risk factors
Many lifestyle-related factors are associated with colorectal cancer. In fact, the link between diet, weight, exercise, and colorectal cancer risk is one of the strongest for any type of cancer.Overweight or obese If you are overweight or obese, you have a higher risk of developing and dying from colorectal cancer than people of normal weight. Being overweight (especially having a larger waistline) increases the risk of colon and rectal cancer in both men and women, but the link seems to be stronger in men.
Do not exercise If you are not physically active, you are more likely to get colon cancer. Therefore, exercising or being more physically active can help reduce your risk.
Certain types of diets Diets high in red meat (such as beef, pork, lamb or liver) and processed meats (such as hot dogs and some canned meats) increase the risk of cancer. colorectal mail.
Cooking meat at very high temperatures (frying, grilling or roasting) creates chemicals that can increase cancer risk. However, scientists have yet to figure out how much this factor can increase the risk of colorectal cancer. And whether other dietary components (for example, certain types of fat) affect colorectal cancer risk.
Smoking People who have smoked for a long time have a higher risk of developing and dying from colorectal cancer than non-smokers. Smoking is a leading cause of lung cancer, but it is also linked to many other cancers.
Heavy alcohol use Colorectal cancer is associated with moderate to heavy alcohol use. Limiting alcohol use to no more than 2 drinks a day for men and 1 drink a day for women can have many health benefits, including reducing the risk of many types of cancer.
Yếu tố nguy cơ ung thư đại trực tràng có thể thay đổi
2. Unmodifiable risk factors for colorectal cancer
Older age The risk of colorectal cancer increases with age. Younger people can also get it, but colorectal cancer is much more common after age 50.Have colorectal polyps or colorectal cancer If you have a history of adenomatous polyps, you have an increased risk of colorectal cancer. This is especially true if you have polyps that are numerous or large in size or if any of them have dysplasia.
If you have had colorectal cancer, even though the cancer has been completely removed, you are still more likely to develop new cancers in other parts of the colon and rectum. The chances of this happening are greater if you had colorectal cancer at a young age.
History of inflammatory bowel disease If you have inflammatory bowel disease (IBD), including ulcerative colitis or Crohn's disease, your risk of colorectal cancer is increased.
IBD is a condition in which the colon has been inflamed for a long time. People who have had IBD for many years, especially if left untreated, often develop dysplasia. Dysplasia is a term used to describe cells in the lining of the colon or rectum that are abnormal, but are not actually cancerous. However, over time, these cells can change into actual cancer.
Family history of colorectal cancer or adenomatous polyps Most colorectal cancers are found in people who do not have a family history of colorectal cancer. However, nearly 1 in 3 people with colorectal cancer have other family members who have had the disease.
People with a history of colorectal cancer in an immediate relative (parent, sibling or child) are at higher risk. The risk is even higher if that relative was diagnosed with cancer when they were younger than 45, or if more than one first-degree relative had it.
The cause for the increased risk is not clear in all cases. Cancer can run in families because genes are inherited, living in the same environment or, in some cases, a combination of risk factors.
Having a family member who has had adenomatous polyps is also associated with a higher risk of colon cancer. If you have a family history of adenomatous polyps or colorectal cancer, talk to your doctor about possibly starting cancer screening before age 45.
Nếu có tiền sử mắc polyps tuyến (Adenomatous polyps) thì bạn có nguy cơ mắc ung thư đại trực tràng
The most common genetic syndromes associated with colorectal cancer are Lynch syndrome and familial adenomatous polyposis, other rare syndromes that can also increase the risk of colorectal cancer. colon.
Lynch syndrome Lynch syndrome is the most common inherited colorectal cancer syndrome. It accounts for about 2% to 4% of all colorectal cancers. In most cases, the disorder is caused by an inherited defect in the MLH1 or MSH2 gene, but changes in other genes can also cause Lynch syndrome.
The cancers associated with this syndrome tend to develop when people are quite young. People with Lynch syndrome can have polyps, but it tends to be only a small number of cases. The lifetime risk of colorectal cancer in people with this condition can be as high as 80%, but this depends on which genes are affected.
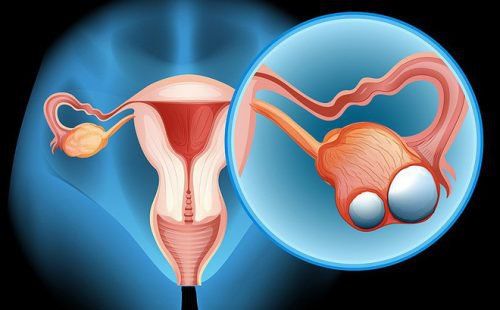
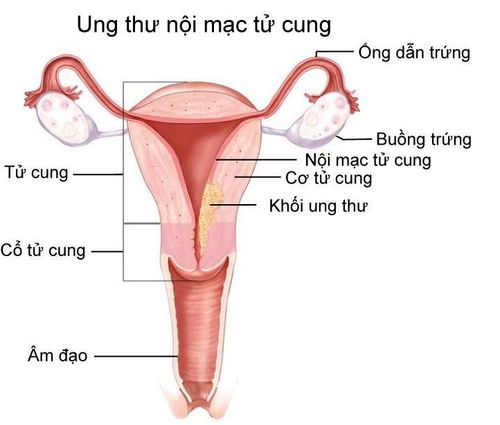
Women with this condition also have a very high risk of endometrial cancer. Other cancers associated with Lynch syndrome include cancers of the ovary, stomach, small intestine, pancreas, kidney, prostate, breast, brain, ureter, and bile duct. Familial adenomatous polyposis (FAP) FAP is caused by changes (mutations) in the APC gene that a person inherits from his or her parents. About 1% of all colorectal cancers are caused by FAP.
In the most common type of FAP, which usually begins between the ages of 10 and 12, people will have hundreds or thousands of polyps growing in the colon and rectum. Cancer usually develops in one or more of these polyps as early as age 20. By age 40, most people with FAP will have colon cancer unless their colon has been removed to prevent cancer. People with FAP also have an increased risk of cancers of the stomach, small intestine, pancreas, liver, and several other organs.
Rare genetic syndromes linked to colorectal cancer
Peutz-Jeghers syndrome (PJS): People with this genetic condition tend to have freckles around the mouth (and sometimes on the hands and feet) and a particular type of polyp called hamartomas in their digestive tract. These people have a much higher risk of colorectal cancer, as well as other cancers, and they are often diagnosed at a younger-than-normal age. This syndrome is caused by mutations in the STK11 (LKB1) gene. MYH-associated polycystic disease (MAP): People with this syndrome develop many colon polyps, which are more likely to become cancerous if not closely monitored with routine colonoscopy. These people are also at increased risk for other cancers of the digestive tract and thyroid. This syndrome is caused by mutations in the MYH gene and is often cancerous in young people. Because many inherited syndromes are associated with colorectal cancer at a young age and are also associated with other types of cancer, it is important to identify families with these inherited syndromes. It allows doctors to recommend specific steps such as screening and other preventive measures in young adults.
Have type 2 diabetes
People with type 2 diabetes have an increased risk of colorectal cancer. Both type 2 diabetes and colorectal cancer share some common risk factors, such as being overweight and being physically inactive. But even after taking these factors into account, people with type 2 diabetes still have an increased risk of colorectal cancer compared with people without diabetes. In addition, these subjects tend to have a worse prognosis after being diagnosed with cancer.
Gastrointestinal cancer screening is a scientific and effective measure for early detection of gastrointestinal cancers (esophageal cancer, stomach cancer, colon cancer) and providing a good treatment plan. best. Currently, Vinmec International General Hospital has a package of screening and early detection of cancers of the gastrointestinal tract (esophagus - stomach - colon) combined with clinical and paraclinical examination to bring the most accurate results. maybe.
When screening for gastrointestinal cancer at Vinmec, you will receive:
Gastrointestinal specialty examination with an oncologist (by appointment). Gastroscopy and colonoscopy with an NBI endoscope with anesthesia. Peripheral blood count (laser counter). Automated prothrombin time test. Automated thrombin time test. Activated Partial Thromboplastin Time (APTT) test using an automated machine. General abdominal ultrasound To register for screening and treatment of gastrointestinal diseases at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register for an online examination. HERE .
References: cancer.org, mayoclinic.org, cdc.gov, cdc.gov