This is an automatically translated article.
Posted by Specialist I Tran Thi Anh Hien - Anesthesiologist - Anesthesiology Department - Vinmec Central Park International General Hospital
Anesthesia is an anesthetic method commonly used when performing surgery and procedures. Anesthesia is generally safe for almost all patients, including those with special medical conditions. However, in some cases, there can be risks when performing surgical anesthesia. Respiratory and circulatory complications may arise as a result of the patient's pre-existing medical conditions, complications from anesthesia, or the invasiveness of surgery.
During anesthesia, anesthetic drugs are introduced into the body through both the respiratory tract and the veins. During anesthesia, the patient completely loses consciousness, is not aware of the surroundings, completely loses pain sensation. The process of anesthesia progresses through stages: pre-anesthesia, induction of anesthesia, maintenance of anesthesia, release of anesthesia (recovery).
1. Respiratory complications in anesthesia
1.1. Bronchospasm
Bronchospasm is a patient with wheezing, stridor, snoring during exhalation, accompanied by rapid breathing or shortness of breath. When the patient is under anesthesia, presenting with difficult artificial ventilation, airway pressure is elevated.
Cause:
There is a history of bronchial asthma. Allergic drugs. Upper respiratory tract irritation by secretions, vomit, blood, and instruments inserted into the pharynx or trachea. Prophylaxis:
Deep and adequate pre-anesthesia for at-risk patients. Induction of anesthesia must ensure deep sleep and spray Lidocaine before inserting the instruments into the pharynx and larynx. Management:
Deep anesthesia with inhalation or intravenous anesthesia. Increase the concentration of O2 in the inhaled air. Use bronchodilators such as Salbutamol, Adrenalin, Corticoid depending on the patient's condition.
1.2. Laryngeal spasms
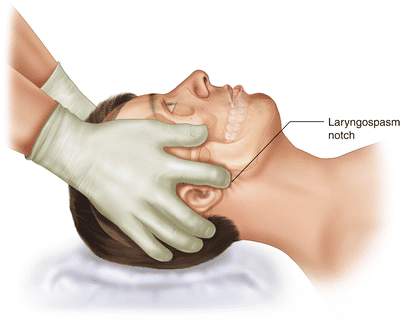
Incomplete laryngospasm: Patient wheezes or wheezes. If the spasm is complete, there is a manifestation of respiratory reverse, not able to ventilate by mask.
Consequences of hypoxia, increased CO2, respiratory acidosis, rapid pulse, high blood pressure, then quickly lead to low blood pressure, slow pulse and cardiac arrest if not treated promptly.
Causes:
Similar to bronchospasm, usually occurs when the upper airway is irritated during superficial anesthesia, increased secretions or bleeding from the upper respiratory tract, inhaled anesthetics have an odor discomfort (dark, spicy), especially when using oropharyngeal interventions such as inserting canules, laryngoscopy for diagnosis or intervention, surgery in the mouth. Stimuli such as peritoneal traction in abdominal surgery Laryngeal spasms are common in children with induction and release of anesthesia. Prophylaxis:
Give the patient 100% O2 a few minutes before induction of anesthesia to increase the O2 reserve in the blood. Spray Lidocaine before placing instruments into the pharynx, trachea. Management:
Put deep sleep with intravenous anesthetic, stop all stimulation. Apply mask and squeeze balloon with 100% O2 if contraction is incomplete. If constriction is complete, release the airway by inserting a large needle into the cricothyroid membrane and squeezing the balloon with 100% O2 through this route. Immediate intubation and combination of extrathoracic cardiac massage if there is circulatory-respiratory arrest. All patients after laryngospasm can be extubated, once the clinical signs have improved, capillary oxygen saturation is continuously monitored and returned to normal values, combined with chest x-ray, blood gas test.
1.3. Lack of blood oxygen
Causes of hypoxia in anesthesia:
Due to inadequate oxygen supply. Reduced ventilation. Change in respiratory-circulation ratio (ventilation-perfusion ratio). Reduced oxygen transport such as anemia, circulatory stagnation, due to cell toxicity. Treatment:
It is necessary to quickly find the cause of hypoxia to treat each specific cause. Initial management is ventilation with 100% FiO2.
1.4. Hypercapnia (hypertension)
Cause:
Decreased ventilation. Bronchospasm. Hemothorax, pneumothorax Endogenous increase in CO2 such as increased metabolism, acid-base disorder, aortic pairing, garot removal, CO2 re-breathing due to ventilator exhalation valve malfunction (damaged valve, misalignment.. .), soda lime is not effective. Exogenous CO2 increase such as CO2 pump in laparoscopic surgery. Treatment:
Adjust respiratory rate and tidal volume. Treat the cause of hypercoaemia
1.5. Upper airway obstruction
Due to sputum sputum, neck hematoma, tongue drop, upper respiratory tract foreign bodies...
1.6. Complications due to endotracheal intubation
Failure due to intubation failure. It is necessary to carefully examine the patient before surgery, assess the difficulty of intubation to prepare in advance.
Injury during endotracheal intubation causes contusion of the lips, broken teeth, bleeding in the oropharynx, damage to the glottis. To prevent and avoid this complication when placing the movement must be gentle, after placement must carefully check by listening to the lungs and measuring CO2 exhaled air.
1.7. Respiratory failure during coma
Causes:
Due to extubation too early when the patient has not been released from anesthesia, the effect of muscle relaxants has not been exhausted, tongue retraction in obese, obese patients, effusion, pleural blood after thoracic surgery due to ineffective suction system, morphine residues, undetected diaphragmatic injury after high abdominal surgery, glottis edema after general anesthesia under prolonged intubation.
Prevention and treatment:
Extubation when eligible. Give the patient oxygen through the mask after extubation, squeeze the balloon

2. Respiratory and circulatory complications
2.1. Lower blood pressure, heart failure
Cause:
Due to the effect of anesthetic agents that cause direct vasodilation or indirect vasodilation, direct inhibition of the myocardium reduces myocardial contractility. Bradycardia due to vagal reflex can lead to to hypotension, even more severe can cause cardiac arrest. Decreased circulating volume due to blood loss, fluid from before surgery, or sudden and massive bleeding. Prophylaxis and management:
For prevention, it is necessary to fully compensate for the lack of circulating volume before performing surgery. Select anesthetic drugs to limit the complications of hypotension for cases of shock, hypovolemia. Place the patient's head low, restore the circulatory volume by means of intravenous fluids, blood transfusions, and use vasopressors when necessary.
2.2. Hypertension
Cause:
The cause is because the patient has a history of diseases such as: hypertension, adrenal tumor, increased intracranial pressure. The patient was intubated while still under general anesthesia, with inadequate analgesia. Increased CO2 and hypoxia. Blood pressure will increase continuously until bradycardia and then drop in blood pressure, which is due to acute myocardial hypoxia. Use of vasoconstrictor drugs (ephedrine, adrenaline), parasympathomimetic agents (pancuronium muscle relaxants, gallamin), high blood pressure return after discontinuation of beta-blockers. Hypertension due to excessive perfusion. Management:
Initiating anesthesia with sufficient depth, spraying lidocaine anesthetic before doing oropharyngeal procedures, maintaining deep anesthesia, good pain relief, performing movements must be very gentle, especially in cases of history of hypertension. Use intravenous antihypertensive drugs as needed.

2.3. Heart arrhythmia
Sinus bradycardia
Cause:
Due to the effect of anesthesia. Irritation of the oropharynx during intubation. History of heart disease, being treated with drugs that slow the heart rate. Lack of circulating volume ... Management:
Stop vagus nerve stimulation. Atropine 0.5-1mg IV dose. Restore missing circulating volume. Reduce the dose of anesthetic you are taking. Sinus tachycardia
Causes:
Lack of circulating volume, shock, pain, hypoxia, excess CO2. Some drugs cause rapid pulse such as muscle relaxants (pancuronium), adrenaline, atropine, ephedrine... Heart rhythm disorders such as atrial fibrillation, atrial flutter, ventricular tachycardia... Treatment:
Treat the causes increase heart rate such as oxygen supply, circulating volume replenishment, pain relief, deep sleep... Use of antiarrhythmic drugs such as beta-blockers, calcium channel blockers, Lidocaine... Extrasystole
Causes:
Pre-existing extrasystoles (NTT). Due to the effect of anesthetics, especially halothan. Increased endogenous catecholamines. Lack of oxygen, excess CO2. Due to hypokalemia ... Management:
If atrial ventricular septal defect is often followed up without treatment. If it is ventricular septal defect, especially double ventricular ventricular arrhythmia, it is necessary to adjust for favorable factors causing the occurrence. Ventricular atrial fibrillation can be used with Lidocaine 1mg/kg by slow intravenous infusion, maintaining 2-4mg/min by intravenous infusion. Complications during anesthesia maintenance
2.4. Increased blood pressure and rapid pulse
This is a common complication when getting out of anesthesia, which can be dangerous for patients with a history of hypertension, coronary artery disease. Prophylaxis: Lidocaine 60 mg endotracheal or 1 mg/kg IV minutes before withdrawal.
The biggest goal of general anesthesia is to ensure patient safety during surgery. Thanks to medical advances, the rate of complications in anesthesia has decreased greatly, currently about 1 in 1,000,000 surgeries. The anesthesiologist will examine the pre-anesthesia to assess risk factors, predict the patient's condition before surgery in order to have a reasonable plan for anesthesia and resuscitation, and closely monitor the patient during and after anesthesia to promptly Time to detect and treat possible complications to ensure patient safety.
Department of Anesthesiology and Anesthesia of Vinmec International General Hospital is one of the departments highly appreciated by patients for its professional quality and care services, helping the patient's treatment and recovery process to be effective. the best.
Apply the world's most advanced technology: The world's most advanced epidural analgesia (ESP) pain relief technique; Anesthesia by ultrasound machine, do not use morphine to relieve pain after surgery. The team of leading experts: The doctors are well-trained and experienced, and are members of the Anesthesiology Associations in Vietnam and Europe. Cooperate with leading professors and experts at domestic and international frontline hospitals to exchange techniques and apply the latest methods of anesthesia and pain relief. Professional - comprehensive patient care: patients are fully and fully consulted before anesthesia and analgesia before and after surgery; apply the program of early recovery after surgery for patients; guide appropriate methods of exercise and rehabilitation so that patients can return to normal activities soon. For more detailed information about methods of anesthesia and pain relief or if you need to be examined and treated at Vinmec International General Hospital, please click the "Contact Us" button on the website, or register for an examination. online.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.