This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Thi Ngoc - General Internal Medicine - Endocrinology - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Hypoparathyroidism is a rare disorder in which the parathyroid glands in the neck secrete low levels of parathyroid hormone (PTH). blood in a significant way, adversely affecting many physiological processes.
1. What is hypoparathyroidism?
Parathyroid hormone works in conjunction with other hormones to regulate calcium, phosphorus, and vitamin D levels in the blood and bones. Hypoparathyroidism is defined as a deficiency of parathyroid hormone (PTH). PTH deficiency can cause a decrease in calcium levels and an increase in phosphorus levels in the bodyCauses of hypoparathyroidism are divided into two groups:
Primary hypoparathyroidism is a condition in which PTH is not produced. full. As a result, the concentration of ionized calcium in the extracellular fluid falls below the upper limit of normal. Secondary hypoparathyroidism is a physiological state in which PTH levels are low in response to a condition that causes hypercalcemia, such as hypomagnesaemia. This cause is very rare and will be mentioned more in the problem of diseases that increase blood calcium. Given that the most common cause of primary hypoparathyroidism is damage to the parathyroid glands during thyroid or neck surgery, DiGeorge syndrome – is an inherited disorder that compromises the development of multiple systems. in vivo, hereditary hypoparathyroidism, autoimmune disease, radiation therapy for cancer. In addition, other conditions that also cause primary hypoparathyroidism include:
Idiopathic hypoparathyroidism: The patient is born without congenital parathyroid tissue Pseudohyperparathyroidism: The patient is still secrete PTH but the body does not respond to the hormone; Usually caused by autoimmune dysfunction.

Suy tuyến cận giáp là tình trạng thiếu hụt hormone tuyến cận giáp (PTH).
2. What is the role of calcium in the body?
Calcium and phosphorus are among the most abundant elements in the human body. Most calcium is stored in bones and teeth. The rest is free-form calcium circulating in the blood stream or in soft tissues.Calcium is important for the normal functioning of almost every physiological process. This is an element that plays a role in nerve transmission, muscle contraction, cell membrane formation and regulation of enzyme activity as well as participating in communication between cells. For example, blood calcium helps to stabilize blood pressure and maintain normal brain function.
In a healthy adult, the amount of calcium inside the cells is lower when compared to the amount of calcium circulating in the blood. This is thanks to the role of hormones such as PTH which help to stimulate cell walls allowing calcium to flow inwards to carry out their functions.
When you have hypoparathyroidism, the low production of PTH causes an imbalance, the calcium level in the blood of the patient will drop significantly. Meanwhile, the serum phosphorus concentration increased. Simply put, low levels of PTH in the setting of hypoparathyroidism disrupts the ratio balance between calcium and phosphorus. With low circulating calcium levels, the body will have the following symptoms of hypoparathyroidism:
Muscle pain or cramps Feeling of tingling, burning or numbness in the fingertips, toes or around the lips Muscle spasms, especially around the mouth Patchy hair loss, dry skin, brittle nails, fatigue, anxiety or depression, menstrual cramps, seizures, children with hypoparathyroidism may have headaches, vomiting, and problems with their breathing. teeth such as weak enamel or underdeveloped teeth.

Suy tuyến cận giáp sẽ phá vỡ sự cân bằng tỷ lệ giữa canxi và photpho
3. How is the relationship between hypoparathyroidism and hypocalcemia?
Liên quan giữa suy tuyến cận giáp và hạ canxi máu như thế nào?
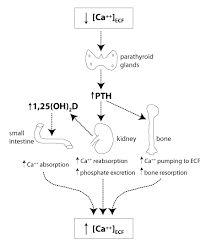
Drawing from timeofcare.com
In parathyroid cells, receptors induce extracellular calcium levels that help regulate PTH production and secretion. If a condition inactivates the extracellular calcium-inducible receptor, it will lead to hypercalcemia. Conversely, activation of these receptors leads to hypocalcemia.
When PTH is released into the blood stream, it participates in the activation of osteoblasts, activates bone resorption leading to bone resorption and the release of ionized calcium into the extracellular fluid, increasing the concentration of calcium in the blood.
Not only that, PTH also has the effect of keeping calcium on the distal tubule in the kidney. PTH-mediated calcium reabsorption is independent of any effect on renal sodium or water reabsorption. This effect of PTH is important in hypoparathyroidism because in the absence of this distal tubular calcium reabsorption, the kidneys waste calcium. This in turn depletes calcium in the intracellular fluid while increasing urinary calcium concentrations.
Besides, PTH stimulates the kidneys to produce enzymes involved in the synthesis of vitamin D. This allows for better absorption of dietary calcium, indirectly increasing blood calcium levels.
Therefore, in the absence of PTH, the body cannot mobilize calcium sources taken from bones, does not reabsorb calcium in the renal tubules or absorb calcium mediated by vitamin D. Therefore, the consequences of deficiency PTH is hypocalcemia, the most common cause of which is primary hypoparathyroidism.
In summary, when the body has symptoms of hypocalcemia, the patient needs to see an endocrinologist to evaluate the function of the parathyroid gland. Although there is no cure for hypoparathyroidism, detecting the disease and using supplements and lifestyle changes will help stabilize the patient's life, reduce the symptoms of hypocalcaemia as well as improve the quality of life. prevent complications.
Master, Doctor Nguyen Thi Ngoc has more than 10 years of studying, researching and working in the field of endocrinology. Doctor Ngoc graduated with a Master's degree in General Internal Medicine from Hanoi Medical University and studied as a Resident Doctor at the University of Lyon (France). Currently, Dr. Ngoc is a treating doctor at the Department of Examination and Internal Medicine, Vinmec Central Park International General Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
MORE:
Guide to supplementing calcium for pregnant women during pregnancy Instructions on how to safely supplement calcium, prevent early musculoskeletal disease Calcium deficiency - the leading cause of osteoporosis and musculoskeletal diseases













