This is an automatically translated article.
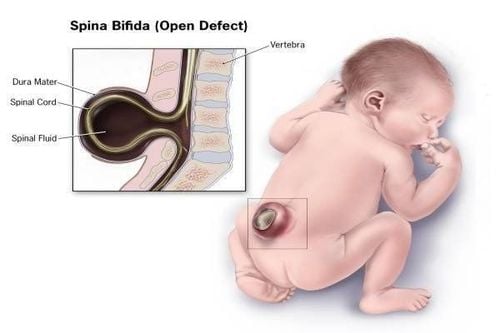
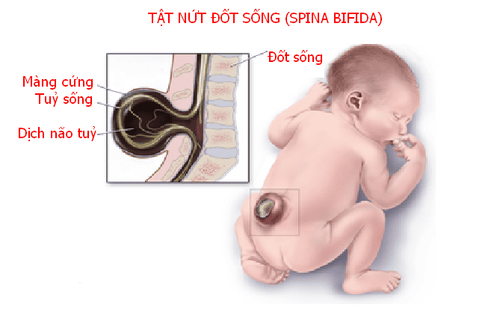
The article is professionally consulted by Master, Specialist Doctor I Nguyen Thi Thanh Binh - Rehabilitation Doctor - Department of General Surgery - Vinmec Danang International General Hospital.Spina bifida or spina bifida is a birth defect that occurs when the spine and spinal cord do not form properly. It falls under the broader category of neural tube defects.
Spina bifida patients have many problems with neurological deterioration, so spina bifida rehabilitation plays an important role in helping patients integrate into the community, avoiding possible complications. happen.
1. Types of spina bifida
The neural tube is the embryonic structure that eventually develops into the baby's brain and spinal cord and the tissues that surround them. In babies with spina bifida, part of the neural tube does not develop or close properly, causing defects in the spinal cord and in the bones of the spine.Spina bifida can range from mild to severe, depending on the defect type, size, location, and complications. Surgical treatment of spina bifida is necessary, although it does not always solve the problem completely.
In general, spina bifida has three main forms (mild to severe):
Hidden spina bifida: An opening in one or more vertebrae (bones) in the spine without obvious damage to the spinal cord. ; Meningeal hernia: The meninges - the protective covering around the spinal cord - pushes out through the opening in the vertebrae in a sac called a meningeal hernia. The spinal cord remains unaffected, which can be repaired with little or no nerve damage; Spinal cord hernia: This is the most severe form of spina bifida, in which part of the spinal cord itself protrudes through the back. In some cases, the bags are covered with leather; In other cases, tissues and nerves are exposed.
2. Goals of spina bifida rehabilitation
The goals are different at each stage of development:At birth, care is more focused on preserving functions and preventing complications, while the child grows up, measures to achieve independence become more important; Newborn (0 - 3 months old): Surgery to close the hernia hole in the spine and control hydrocephalus. Basic assessment of neurosurgery, orthopedic surgery, urology, and rehabilitation; Infants (3 - 18 months): Normal intracranial pressure and central nervous system function are maintained, best cognitive function is preserved. Muscles and bones are maintained in function for optimal development Control urinary tract infections ; Toddlers (18 months - 3 years old): Continue to take care of bowel problems, optimize mobility, prevent latex allergies, implement an early intervention program; Pre-school age: Continuing care, determining the appropriate pre-school program, continuing the overall development of the child; School age: Rehabilitation so that children can be independent in handling defecation, using splints, and taking care of their skin. Children make friends and engage in recreational activities, identify and treat precocious puberty; Youth: Independent in self-care, receiving full employment/educational services, being a manager in the prevention of complications, knowledgeable about folic acid use. Be aware of sexual problems; Adults: Find work, get support services, get fertility information, transition to intensive care.
3. How is spina bifida rehabilitation?
Neurological deterioration is a potential complication of spina bifida, which can adversely affect the patient's ability to be independent and lead to problems such as pressure ulcers and bladder problems. nervous system, nervous gut... The rehabilitation is different in each case.3.1 Pressure ulcers Patients with spina bifida are very susceptible to chronic skin lesions such as wounds to the buttocks and lower extremities. Pressure ulcers are the most common cause of skin damage as a result of prolonged sitting or wearing a brace. Because most children with spina bifida have incomplete anal and urethral contractions, they face many difficulties with the problem of skin rash when wearing diapers for a long time. During the life of a person with spina bifida, one of the most important issues to consider is the prevention of pressure ulcers.
Commonly used preventive measures are:
Keep the child as dry and clean as possible, but often unsatisfactory due to urinary incontinence. Children lose sensation in the lower body, so there are no signs that the patient needs to change position or reduce pressure on a part of the body. For ulcer prevention, performing orthopedic procedures and wearing appropriate orthopedic appliances should be considered. As a child learns to walk, pressure on pressure points in the feet can lead to pressure sores or calluses. If orthopedic devices are recommended, pressure points should be checked regularly, especially at the beginning of use or when the appliance is newly built. Ulcer monitoring: Pressure injuries can occur in older children with kyphosis or scoliosis who are wheelchair-bound and have poor balance in their seats. Parents or caregivers should be instructed to monitor these areas at least twice daily. Change position: In case of scarlet fever, the child should lie on his or her stomach until the skin redness disappears. Teach children to change their sitting positions frequently. The use of special mattresses and modified wheelchair seats can also be of great help in ulcer prevention. During the school years, children should learn to monitor their own skin conditions. Before entering the bath, check the water temperature with your hands. After bathing, at least every night, pressure areas such as feet and buttocks should be photographed with a phone to check. When a pressure ulcer occurs, the first treatment is to keep the ulcer area free of pressure, clean, and dry. For grade II ulcers, just the above treatment is enough. However, when the skin lesions are thick and large, they are slow to heal and often require plastic surgery such as flaps. Pressure ulcers can cause osteomyelitis, a complication that is difficult to manage successfully.
3.2 Neurogenic Bladder The bladder in children with spina bifida presents with varying degrees of sphincter dysfunction, called neurogenic bladder. However, there is a high probability that nerve damage will develop over time.
At birth, the majority of patients have a normal upper urinary tract, but nearly 60% of them will have impaired upper urinary tract function due to infection, bladder changes and reflux.
The foundation for the best management of bladder sphincter dysfunction is early detection, catheterization, and active therapy. In the long-term prognosis of patients with vesico-sphincter loss, it is important that management begin before the consequences of bladder dysfunction become apparent.
3.3 Nervous Intestine In the disease of the spinal canal, which is not closed, when the nerve is damaged, it will lead to problems of the affected intestine such as: bowel incontinence, constipation, digestive disorders... The goal of treatment is regular bowel cleansing and proactive bowel control by establishing a bowel care program that is tailored to each child's needs. Specifically:
It is recommended to follow a nutritious diet, containing a small amount of fiber and drink enough water to keep fluid balance. As children begin to regulate behavior, toilet training is very important. Usually rectal suppositories are used to help a child pass stools, however some parents and children find it more comfortable to use their fingers to stimulate bowel movements instead of using rectal suppositories. As children grow up, they will be instructed to wash the anus. Because of poor anal sphincter tone that makes it difficult for a child to hold stools, using a ball or cone can help seal the lower rectum when an enema with warm tap water is added. Anal irrigation is the most important treatment for neuroenteric conditions today. Frequent irrigation reduces the risk of stool leakage and has a positive effect on sphincter tone and rectal volume.

3.4. Musculoskeletal conditions in patients with spina bifida Typical congenital malformations in patients with spina bifida are kyphosis, congenital hip dislocation, hip flexor contracture and foot deformity crooked, heel-concave feet, and vertical talus. Developmental malformations include scoliosis, lumbar spine overextension, hip and knee flexion contractures, extra-knee rotation deformity, hip and tibial malrotation, and neck and table deformity. legs like a horse's foot, the foot is bent inward and the flat foot is crooked. Treatment:
The treatment strategy should take into account the growth of the spine. We should also consider delaying orthopedic surgery, which can lead to an unsatisfactory correction. Because spinal deformities are always progressive, spinal deformities combined with skin and soft tissue disorders can lead to secondary problems, such as pressure ulcers. Even mild scoliosis can affect balance and impair a child's ability to walk and sit. As the curve progresses, a diagonal pelvis may appear, followed by pressure ulcers.
The main reasons for surgery are the prevention of further deformity, the creation of a stable and balanced spine, the prevention of secondary complications (eg, pressure ulcers, pulmonary dysfunction) and the improvement of balance. equal to sitting. Surgery should not be indicated for the purpose of improving walking, and should be aware that minimal mobility may be lost after spinal correction surgery.
3.5. Hip deformity Monitor hip condition to prevent hip dislocation and slippage. It is important to maintain a comfortable sitting position, to avoid pain, and to prevent secondary problems such as crossed pelvis, contractures, scoliosis, and pressure ulcers. Therefore, prevention of hip contracture is a key intervention. Current treatment goals are based on functional research findings, with a focus on maintaining range of motion of the hip by releasing contracture. 3.6. Foot deformity Because the muscles of the leg are innervated by the lower spinal cord, about 95% of people with spina bifida will develop a deformity of the foot, which can include heel spurs, ponyfoot, or crooked feet. , crooked feet, curved feet combined with deformities. Some cases of deformity are mild and do not require surgery. More severe cases require surgery
Early intervention with physical therapy such as a cast, brace or surgery can help prevent fixed bone deformities. Initial treatment for all deformities includes passive stretching or manipulation exercises and then splinting. Deformities such as clubfoot, mild inversion, or postural heel deformity may respond to passive manipulation alone.
Only cases of incomplete torticollis should be cast between passive manipulations, and then monitored by an experienced therapist, as pressure ulcers can occur.
Even with early intervention, recurrence is common, at which time surgical release of contracture, tendon transfer, and bone orthopedics are often necessary. Stimulant surgery of the foot (subtalar or trigeminal hardening) is not recommended because there is a high risk of foot ulceration even if the deformity is corrected.
Surgical correction of severe deformities such as clubfoot or vertical talus, if necessary, should wait until the child has grown to the stage where he can stand upright. To minimize the possibility of recurrence of the deformity, the correct-sized orthotic device should be worn immediately, and the child should be encouraged to stand and walk with the orthopedic device.
3.7. Psychology, learning and communication Many people with spina bifida/hydrocephalus have learning difficulties. The sooner these problems are identified, the sooner a resolution strategy can be put into practice. Understanding how children learn will help professionals participate in planning for children's education and health care.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.