This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalGastroesophageal reflux disease is increasingly common in Asian countries. The frequency data are mainly based on the survey of the frequency of typical reflux symptoms in the community and the frequency of reflux esophagitis (reflux esophagitis) on endoscopy. Studies noted that the incidence of reflux esophagitis in Singapore increased markedly while the prevalence of H. pylori infection gradually decreased during the 10-year follow-up period.
1. Frequency of reflux esophagitis and frequency of peptic ulcers in Vietnam
Vietnam, studies performed at the same hospital in HCMC. HCM over a period of 15 years showed an increased frequency of reflux esophagitis while the frequency of peptic ulcers decreased markedly. However, until recently, there were no studies in the country that revealed the true prevalence of reflux esophagitis and the association between reflux esophagitis and H. pylori infection in untreated patients. upper gastrointestinal symptoms.
In 2014, author Quach Trong Duc, conducted a study on 203 patients with upper gastrointestinal symptoms and performed gastrointestinal endoscopy on patients at Ho Chi Minh City University of Medicine and Pharmacy Hospital. Chi Minh, aimed at (1) Determining the frequency and severity of reflux esophagitis; and (2) determine the association between reflux esophagitis and H. pylori infection in patients presenting with untreated upper gastrointestinal disease. The author found: The rate of reflux esophagitis in patients with untreated upper gastrointestinal symptoms was 10.9%, of which 1% was associated with peptic ulcer. All cases of reflux esophagitis were mild. There is a statistically significant inverse relationship between H. pylori infection and reflux esophagitis.
2. Rate of reflux esophagitis and peptic ulcer disease
According to the above study by author Quach Trong Duc, the rate of reflux esophagitis was 10.9% and the rate of peptic ulcer was 11.9%. Data from a study sampled in 2011 by the same author at the same hospital showed a higher rate of reflux esophagitis (16.9%) and a lower rate of peptic ulcers (6. %).
Another feature is that all cases of reflux esophagitis recorded in this study were mild, while domestic studies performed at back-line hospitals showed a higher incidence of esophagitis. Reflux severity ranges from 1.9 to 5.9%. This can be explained because the patient population in the previous studies included those who had been treated in frontline hospitals but had not been successful.
Reflux esophagitis tends to recur on discontinuation of the drug, especially in severe cases of reflux esophagitis. Meanwhile, the incidence of peptic ulcers (with the most common cause being H. pylori) tends to decrease once eradication is successful. It is not surprising, therefore, that statistics in upper-level hospitals tend to show higher rates of reflux esophagitis while rates of peptic ulcers are lower compared with medical units. At the same time, the rate of severe reflux esophagitis in the back-level hospitals will also be higher. When reviewing the domestic literature, the authors have not recorded any studies showing actual data at primary health care levels.
3. Relationship between Helicobacter pylori infection and endoscopy disease forms
Research results of author Quach Trong Duc showed that the prevalence of H. pylori infection in gastric ulcer and duodenal ulcer patients in this study was 80% and 94.1%, respectively, and when calculated as a whole, it was 90, 9%. Thus, although research in some countries recently noted that the rate of peptic ulcers not caused by H. pylori tends to increase, the current data in our country shows the infection rate. H. pylori in peptic ulcer disease is almost unchanged from before.
Therefore, in cases where patients with peptic ulcers are detected on endoscopy but the results of the diagnostic test for H. pylori (-), it is necessary to carefully consider the false-negative factors of H. pylori. diagnostic method and, where necessary, may need to be combined with a second H. pylori diagnostic method.
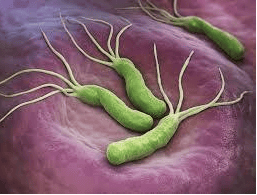
4. H. pylori infection associated with reduced risk of reflux esophagitis
In this study, the author found that H. pylori infection was associated with a 5-fold reduction in the risk of reflux esophagitis. This is the first study in the country to show this association. Some previous studies in other communities also showed an inverse association between H. pylori infection and reflux esophagitis. Chung et al. (2011) performed a case-control study that matched age and gender in 5616 health check-up cases with upper gastrointestinal endoscopy and diagnosis of H. pylori infection by serologic testing. study in Korea. The results of this study show that the frequency of H. pylori infection in the group of patients with reflux esophagitis is lower than that of patients without reflux esophagitis (38.4% vs 58.2%, p <0.001 The rate of H.pylori infection in the group with severe reflux esophagitis was also lower than in the mild reflux esophagitis group (22.4% in the group with grade C and D reflux esophagitis, compared to with 34.3% in groups A and B, p<0.001).
5. Patients with reflux esophagitis have a milder degree of atrophic gastritis than the group of patients without gastroesophageal reflux disease.
Shirota et al. (1999) recorded in Japan the prevalence of H. pylori infection in patients without gastroesophageal reflux disease, mild reflux esophagitis, and severe reflux esophagitis. The difference was statistically significant, decreasing gradually in 3 groups with the rates of 60.7%, 47.8% and 14.8%, respectively (p < 0.05).
Shirota's study also showed that the group of patients with reflux esophagitis had a milder degree of atrophic gastritis than the group of patients without gastroesophageal reflux disease. This is explained by the fact that H. pylori infection increases the rate of atrophic gastritis. As a result, gastric juice will be less acidic, so it is less likely to damage the lining of the esophagus even if it is refluxed into the esophagus.
Some studies also show that this association is more pronounced when considering the CagA-producing H. pylori strain alone. The H. pylori CagA (+) strain is toxic and has a high risk of causing gastritis. Once gastritis occurs, parietal cell damage in the body region results in decreased acidity of gastric juice. Although in the author's study Quach Trong Duc did not evaluate the genotype of H. pylori, domestic research showed that more than 90% of H. pylori strains in Vietnam are CagA strains. This contributes to our finding of an association between reflux esophagitis and H. pylori infection in this study.

6. Should H. pylori be eradicated if detected in patients with gastroesophageal reflux disease?
A question for the clinician is whether H. pylori should be eradicated or not if detected in a patient with gastroesophageal reflux disease. Wu et al. (2004) noted that after eradication of H. pylori, gastroesophageal reflux disease became more difficult to control, probably due to the restoration of parietal cells in the body region. produce more gastric acid secretion.
However, we all know that in fact in Vietnam the most common malignancy of the upper gastrointestinal tract is gastric cancer, not adenocarcinoma of the esophagus. Moreover, infection with CagA-producing H. pylori strain is associated with a higher risk of gastric cancer while most cases of gastroesophageal reflux disease in Vietnam and Asian countries in general cause symptoms but rarely cause serious complications.
The recent European Maastricht IV consensus also recommends that long-term treatment with proton pump inhibitors in patients with gastroesophageal reflux disease have H. pylori infection but are not on eradication. can aggravate gastric mucosal atrophy - a precursor to gastric cancer. Therefore, it is the authors' opinion that H. pylori eradication therapy should still be recommended in patients with gastroesophageal reflux disease, especially when the need for long-term proton pump inhibitor therapy is anticipated. .
Conclusion
The rate of reflux esophagitis in patients with untreated upper gastrointestinal symptoms is 10.9%, of which 1% is associated with peptic ulcer. All cases of reflux esophagitis were mild. There is a statistically significant inverse relationship between H. pylori infection and reflux esophagitis.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, short bowel syndrome, chronic diarrhea, Crohn's disease , misplaced gastric mucosa in the esophagus, reflux esophagitis...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to treatment patients, customers can rest assured with gastroscopy and esophagoscopy services at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.