This is an automatically translated article.
Posted by Doctor CKII Pham Thi Khuong - Pediatric Center - Vinmec Times City International Hospital1. What is rat-bite fever?
Rat-bite Fever (RBF) is a rarely diagnosed, systemic illness caused by infection with Streptobacillus moniliformis, Streptobacillus notomytis, or Spirillum except S. moniliformis that causes most cases in the United States. Spirillum minus is known mainly in Asia as Sudoku disease, although it can be present worldwide. Infection with S. notomytis has been rarely reported.According to the etiological and clinical etiology we distinguish:
Sudoku disease, described by Japanese authors, is caused by Spirillum minus. Haverhill fever, described by an American author, is caused by an infectious Streptobacillus moniliformis that can be transmitted by the bite or scratch of an animal of the rodent order, especially a mouse, or of certain domestic animals (such as dogs). , cats...) or ingesting food or water contaminated with infected rat droppings. Without early diagnosis and proper treatment, rat-bite fever can cause severe illness and death.

Sốt chuột cắn (Rat-bite Fever- RBF) là một bệnh hiếm khi được chẩn đoán
2. Epidemiology
In the United States, rat-bite fever is commonly caused by S. moniliformis. The disease is very rare, with only a few cases reported each year. For example, between 2000 and 2012, only 17 cases were identified in California.The risk of contracting rat-bite fever by S. moniliformis after a rat bite has been reported to be 10% and currently includes pet store employees and laboratory technicians who are susceptible because rats have become pets and popular research subjects.
In Asia, rat-bite fever is called sodoku (hence : rat and doku : poison) and it is mainly caused by Spirillum minus . S. notomytis has also been reported in Japan. This species was originally isolated from a spinifex gerbil in 1979 and genetically described in 2015.
3. Transmission process
S. moniliformis is commonly found in the nasal and pharyngeal flora of rats and perhaps other rodents. Most rats show no symptoms; however, they can sometimes demonstrate signs of disease. The incidence of nasal transmission of S. moniliformis (even in healthy laboratory rats) is quite variable, reported to be as high as 100 percent.S. moniliformis infection can result from a bite or scratch from an infected or infected rat or from handling rats at home or work (eg, lab or pet store) . The risk of infection after a rat bite has been reported to be as high as 10%. Transmission can also occur by oral contact, such as kissing a pet rat.
S. moniliformis infection can also occur after ingesting food or water contaminated with infected rat droppings. When infection occurs through this route, it is called "Haverhill fever"; The name is named after an outbreak in 1926 when 86 people in Haverhill, Massachusetts fell ill with fever after consuming contaminated unpasteurized milk. A similar outbreak occurred in 1983 in 304 boarding school students in Chelmsford, England. Haverhill fever was described in India 2000 years ago and it is more common than Sudoku disease.
The mode of transmission of S. minus, S. notomytis and S. moniliformis is similar; however, S. minus and S. notomytis infections are not associated with contaminated food or water.

S. moniliformis thường được tìm thấy trong hệ thực vật mũi và hầu họng của chuột
4. Clinical manifestations
The clinical manifestations of rat-bite fever depend on the causative organism (S. moniliformis or S. minus ).4.1 S. moniliformis The clinical manifestations of RBF due to S. moniliformis can range from a mild flu-like illness to fulminant sepsis in children and adults. The mortality rate of rat-bite disease is about 13 percent in untreated patients.
The incubation period is usually less than 7 days. Sudden high fever with muscle pain, moving joint pain, vomiting, sore throat and headache. Symptoms are intense, but bites or scratches are usually not inflamed. People with gastrointestinal rat-bite fever experience more severe vomiting and often a sore throat than those who contract the disease through bites. The rash is commonly seen on the extensor surfaces of the extremities and may involve the palms and soles. Although usually maculopapular, it can be petechiae, vesicular nodules, or purpura. Initial symptoms are usually followed by rash followed by polyarthritis in 50% of patients. Arthritis is most commonly found in the knee joint, followed by the ankle, elbow, wrist, shoulder, and hip. The presentation of arthritis can vary, but the majority of cases are multi-joint, and in some, the distribution is asymmetrical. Although symptoms may clear up on their own without antibiotic treatment, in some cases, fever can recur and arthritis can persist for several years. In the case report of a child with swollen knees, pathogenic bacteria were found to persist in the joints for months despite the eradication of bacteremia and other sites.
4.2 S. minus In contrast to S. moniliformis infection, S. minus has a longer incubation period (one to three weeks). In addition, the original wound may reappear at the onset of systemic disease or persist with edema and ulceration with associated congenital disease. About 50 percent develop a central hemorrhagic rash. Arthritis is uncommon.
4.3 S. notomytis S. notomytis presents with fever, rash and polyarthritis
5. Complications of rat-bite fever
Sepsis is the most common complication in the Chelmsford and Haverhill outbreak. Other serious complications include meningitis, endocarditis, myocarditis, pneumonia, focal abscess, septic arthritis, and chronic osteoarthritis.Endocarditis is a well-described complication. Individuals often have a history of valvular disease and symptoms similar to endocarditis from other causes, including the presence of anemia, Osler nodes, and hepatosplenomegaly. In a case series, the mortality rate associated with endocarditis due to S. moniliformis was 53%.
Blood tests: Moderately elevated white blood cell count and elevated erythrocyte sedimentation rate in some patients
Joint effusion: Culture of joint fluid detects bacteria. The amount of fluid varies between joints.
Nhiễm khuẩn huyết là biến chứng phổ biến nhất
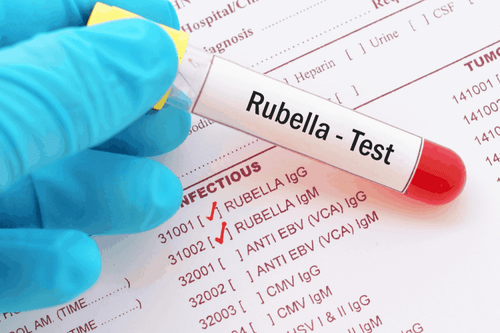
6. Diagnosis of rat-bite fever
Rat bite fever (RBF) is often diagnosed empirically because cultures cannot be found for S. moniliformis or S. notomytis and S. minus . No serological tests are available; however, 16S rDNA gene sequence analysis alone has been used for diagnosis on appropriate specimensEmpiric diagnosis Diagnosis is based on patients with unexplained fever or sepsis and history of exposure to rats or being bitten by rats. Particular attention is given in patients with recurrent or intermittent fever pattern, maculopapular rash and/or polyarthritis or polyarthralgia (usually involving the knees and ankles).
Definitive diagnosis A definitive diagnosis is extremely difficult if thought to be caused by S. moniliformis or S. notomytis:
Specimen: Blood, synovial fluid or fluid from an abscess
16S rDNA test ( if available) on appropriate specimens such as tissue (valvular, bone) or synovial fluid may be helpful in the diagnosis of S. moniliformis or S. notomytis. However, clinical utility and sensitivity have not been demonstrated. This type of test is not available on regular blood samples.
Differential Diagnosis The differential diagnosis for a patient presenting with some combination of fever, maculopapular rash, and/or polyarthritis is broad and involves a variety of infectious organisms. These agents can usually be diagnosed through the available culture, serological, and molecular techniques. It is important to obtain a recent travel and/or exposure history to help prioritize potentially infectious organisms. Detailed discussion of how to diagnose these infections is discussed separately in the relevant topic reviews.
Fever and other rash:
Viral: There are several viral causes that should be considered in a patient with fever and rash. These mainly include enteroviruses, measles, parvovirus, HIV, dengue, lymphocytic pleurisy virus, and Epstein-Barr virus. Infection with these viruses should be considered in patients with an appropriate history of activity and/or exposure. For example, enterovirus infections are common in children. These infections are usually diagnosed through serologic testing or polymerase chain reaction (PCR
Bacterial: Bacterial causes presenting with a hemorrhagic rash include endocarditis caused by Staphylococcus aureus or Streptococcus pyogenes). , as well as disseminated gonorrhea and meningococcal disease. These infections are usually diagnosed through positive blood or fluid cultures.Patients with Salmonella typhi present with pale spots (pink spots) and people with toxic shock syndrome caused by a S. aureus or Streptococcus infection are more likely to have diffuse erythema
Spirochetal : A spirochete infection that presents as a rash that can be polycythemia vera or haemorrhage, as seen in secondary syphilis, leptospirosis, and recurrent Borrelia fever
Other tick-borne diseases : Tick-borne pathogens can cause a macular, maculopapular, or hemorrhagic rash as shown seen in infections caused by Rickettsia rickettsii (the causative agent of Rocky Mountain Spotted Fever), typhi Rickettsia, and less commonly
Polyarthritis: Parvovirus or disseminated gonococcal infection are possibilities in patients with polyarthritis plus fever and rash. For patients with more localized joint results, septic arthritis due to staphylococcal and streptococcal strains should be considered.
7. Treatment of rat-bite fever

Nguyên tắc điều trị bệnh là chăm sóc vết thương tại chỗ và sử dụng kháng sinh
Treatment of animal bites Incidence of more than 25% of untreated patients. The treatment of rat-bite fever is combined with rat bite care. Wound care includes cleaning the wound and getting a tetanus shot. Rats and other rodents are not infected with rabies virus and there have been no reports of transmission of rabies virus to humans from this group of animals.
Penicillin antibiotic treatment is the treatment of choice for people with rat bites, and prompt treatment can prevent serious complications. The mortality rate of the disease is about 13 percent in untreated patients. Empiric treatment should be initiated immediately in patients with clinical manifestations and factors associated with rat bites, or in their possession or care.
Uncomplicated forms include fever, myalgia, polyarthritis, polyarthritis, vomiting, headache and/or rash. In these individuals, the total duration of treatment was 14 days. Most patients are initially treated with intravenous antibiotics. If there is a significant improvement in symptoms after initial treatment, then the oral route will be switched to the full course of treatment.
Penicillin or ceftriaxone are antibiotics of choice.
For adults and children who cannot take beta-lactam antibiotics, tetracycline can be given ceftriaxone.
Streptomycin and gentamicin as alternative agents; however, their use is limited due to nephrotoxicity
Adults: IV penicillin (2 million units every 4 hours) for 5-7 days, continue treatment if clinical improvement with ampicillin (500 mg/4 times) /day) orally for 7 days. If the patient is allergic to penicillin, tetracycline (500mg orally 4 times a day) or doxycycline 100mg twice a day can be used.
Children: Intravenous penicillin (20,000-50,000 units/kg/day divided into 6 times/day), maximum dose 1.2 million units/day. For pediatric patients with no indications for hospitalization, treatment with penicillin V (25mg/kg/day orally 3-4 times/day). Treatment lasts 7-10 days. For pediatric patients allergic to penicillin, severe clinical condition, can be treated with doxycylin. Although tetracycline has a side effect of causing tooth discoloration in children, this side effect is very small for short-term doses. For children weighing over 45kg, the same dose can be used as adults. Younger children dose 2-4mg/kg divided into 2 times/day. Streptomycin can be used to treat both adults and children, although there are some barriers to its use such as toxicity, family requirements or some pharmacies do not have it.
Follow-up In patients with possible serious complications, response to treatment must be carefully assessed and treated more aggressively (eg, higher or prolonged intravenous antibiotics) if the patient does not have Clinical signs improved.
Complications from rat bites are very rare. But if present are meningitis, endocarditis, myocarditis, pneumonia, localized abscess, sepsis, pyogenic arthritis and multi-organ failure. Although mortality is up to 50 percent, the majority of these occur when antibiotic treatment is ineffective.
For patients with severe complications of endocarditis or for patients with prosthetic valve involvement, higher doses of penicillin and an aminoglycoside combination should be considered, similar to the treatment of endocarditis due to endocarditis. other streptococcus.).
In both adults and children allergic to penicillins and cephalosporins, treatment with doxycycline can be performed at the doses described above.
Adults: Penicillin G intravenously (12-18 million units daily either continuously or in four or six equally divided doses) for four weeks. For penicillin-insensitive isolates, the dose may be increased to 24 million units per day either continuously or in four or six doses. An alternative to penicillin is ceftriaxone at 2 grams/day for 7 to 10 days.
Children: For children with complications, give penicillin G intravenously (200,000 to 300,000 units per kilogram per day in four divided doses for up to 24 million units per day) for four weeks.
For patients suitable for conversion to outpatient intravenous therapy, intravenous ceftriaxone (50 to 100 mg/kg daily, up to 2 grams/dose) may be used as an alternative. for intravenous penicillin.
8. Prevention of rat-bite fever

Những người nuôi chuột không nên hôn hoặc liếm chúng
Educate on the signs and symptoms of rat-bite disease to raise awareness to help prevent serious illness in people exposed to rats. In addition, after a rat bite, it is reasonable to administer penicillin V for three days (adults: 500 mg four times daily; children: 25 to 50 mg/kg daily in three or four divided doses, up to 2 grams per day). However, the effectiveness of antibiotic prophylaxis is still unknown.
9. Some points to note
Rat-bite fever is often clinically diagnosed because culture for S. moniliformis is difficult and S and serological testing is not available. However, 16S rDNA gene sequence analysis was used for diagnosis on appropriate specimens.The treatment of patients with rat bites includes topical wound care in those bitten by rats and antibiotics. Penicillin is the treatment of choice, and prompt treatment can prevent serious complications. Empiric therapy should be initiated in patients with a compatible clinical presentation and exposure history, as testing is difficult and may take several days to obtain results.
To prevent infection after a rat bite, a three-day course of oral penicillin V (adults: 500 mg four times daily; children: 25 to 50 mg/kg daily in three or four divided doses, max. 2 grams per day) is reasonable; however, the effectiveness of antibiotic prophylaxis is unknown.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Reference Rat-bite fever (RBF).Page last reviewed: January 18, 2019.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP) Rat bite fever. Katherine Yudeh King, MD, PhD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: May 2020. | This topic last updated: Jan 20, 2020. 3. Trinh Ngoc Phan, Infectious Diseases, Medical Publishing House 1983.
SEE MORE
After being bitten by an animal, do you need a rabies vaccination? Identifying early signs of rabies in humans List of 5 rabies vaccines circulating in Vietnam
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.