This is an automatically translated article.
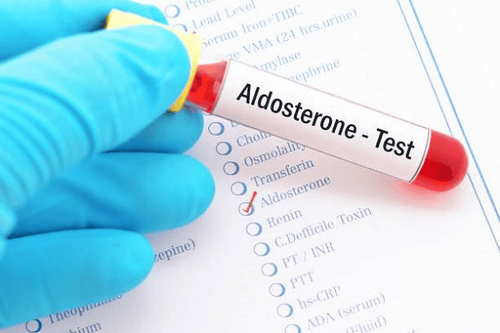
Hypoaldosteronism is a kidney disease, it directly affects human health. So let's learn the most basic information about pseudo-aldosteronism syndrome for timely examination and treatment.1. What is Aldosterone?
Aldosterone is a salt-metabolizing corticosteroid (mineralocorticoid) secreted by the adrenal cortex. The release of aldosterone is mainly controlled by the renin-angiotensin-aldosterone system. Decreased extracellular fluid will lead to decreased blood flow to the kidneys, which will stimulate the kidneys to produce and excrete renin. Renin acts on angiotensinogen to form angiotensin I. In the presence of angiotensin-enveloping enzyme (ACE), angiotensin I is converted to angiotensin II. Angiotensin II causes the adrenal cortex to increase production of aldosterone.Aldosterone acts in the distal convoluted tubules, where it increases sodium and chloride reabsorption and also increases the excretion of potassium and hydrogen ions. The result of these effects is increased water retention and increased extracellular fluid volume. The final effect of the change in aldosterone levels is to participate in the regulation of blood pressure.
2. Aldosterone reduction pseudoclassification
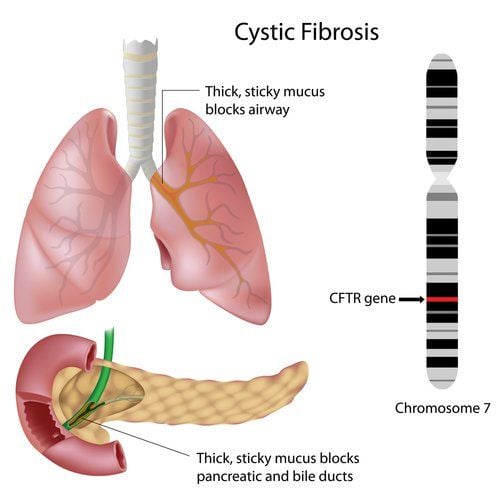
2.1. Pseudo-hypoaldosteronism syndrome type 1 - recessive inheritance Pseudohyperaldosteronism type I is autosomal recessive and tends to be persistent. Sodium channels in extra-adrenal tissues can be affected, leading to rashes or complications similar to cystic fibrosis. Manifestations of this syndrome can include low blood pressure, low blood sodium, and increased potassium levels. The main cause is because the kidneys store too much potassium, but when excreted, it is excreted as water and sodium.
2.2. Pseudo-hypoaldosteronism syndrome type 1 - inherited dominant gene For children born with pseudo-hypoaldosteronism syndrome - the dominant gene will have a resistance to mineral salt coricoids. Autosomal dominant inheritance of suicide is usually less severe, primarily affects the mineralocorticoid receptors in the kidneys, and may be in remission to some extent in children.
2.3. Pseudohypoaldosteronism syndrome type 2 Pseudohypoaldosteronism syndrome is a very rare syndrome and usually occurs in patients with one of the following conditions:
Fanconi syndrome People with myelodysplastic nephropathy Exposure to medications various (usually acetazolamide, sulfa, ifosfamide, tetracycline or expired streptozotocin) Type 2 hypoaldosteronism is due to decreased bicarbonate reabsorption in the proximal tubule, if plasma bicarbonate concentration is normal then urine pH > 7; If plasma bicarbonate concentration is decreased due to intermittent loss, urine pH is <5.5. This syndrome may be part of systemic dysfunction of the proximal tubules, with patients having increased excretion of glucose, uric acid, phosphorus, amino acids, citrate, calcium, potassium, and protein. Osteoporosis or osteomalacia (including rickets in children) may be present and progressive. Possible mechanisms include hypercalciuria, hyperphosphaturia, impaired vitamin D metabolism, and secondary hyperparathyroidism.

Giảm aldosterone có mối liên quan với tình trạng cường cận giáp thứ phát
3. What to look out for before testing for hypoaldosteronism?
Factors that can affect test results include:
Excessive exercise and stress can stimulate the adrenal cortex to secrete and increase aldosterone levels. Hormone values may vary due to posture, position, diet, daily changes and pregnancy. If radiation therapy is used for the test, recently taken radioactive drugs will affect the test results. Drugs that can cause elevated levels include diazoxide, diuretics, hydralazine, laxatives, sodium nitroprusside, potassium, and spironolactone. Medications that can lower actual aldosterone levels include angiotensin-converting enzyme inhibitors (such as captopril), fludrocortisone, propranolol, and licorice.
4. Before testing for pseudo-hypoaldosteronism syndrome, what should the patient do?
Before performing the aldosterone test, the patient needs to take some notes for the most accurate test results.
Let your mind be in a natural and relaxed state. Some patients may panic and need a lot of psychological support. You need to prepare your diet, maintain a normal salt diet (about 3g/day) for at least 2 weeks before blood or urine samples are taken. You should tell your doctor about any medications you're taking so they can advise you to stop taking any that could affect the test results. If these medications are stopped at least 2 weeks before a blood or urine test, the results will be more accurate. Do not take a renin inhibitor (such as propranolol) 1 week before the test. Because of aldosterone-like effects, avoid licorice for at least 2 weeks before the test.
Bệnh nhân cần tránh một số thức ăn, chất gây ảnh hưởng đến kết quả xét nghiệm aldosterone
5. Steps to perform the aldosterone test
A mock test for a baseline aldosterone reduction will take place as follows:
Use a string, elastic or special device to tighten around the upper arm to temporarily stop the blood circulation Get a new, iron needle with the same blood collection site with alcohol Directly draw blood from a vein and attach a tube to allow the blood to flow back out. Stop when enough blood is drawn and immediately apply urgo to the injection site. Hypoaldosteronism is a kidney disease, it directly affects human health. Thoroughly learning information about this syndrome will help you to have timely examination and treatment.
Follow Vinmec International General Hospital website to get more health, nutrition and beauty information to protect the health of yourself and your loved ones in your family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.