This is an automatically translated article.
The article was professionally consulted with Specialist Doctor I, Resident Doctor Nguyen Hung Tien - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Hai Phong International General Hospital.Acute liver failure in children is a rare but serious condition. The initial symptoms are often similar to common childhood illnesses, while the progression is very rapid, and can sometimes be life-threatening. So parents, families, and even pediatricians may not realize it at first until it's advanced.
1. What is acute liver failure in children?
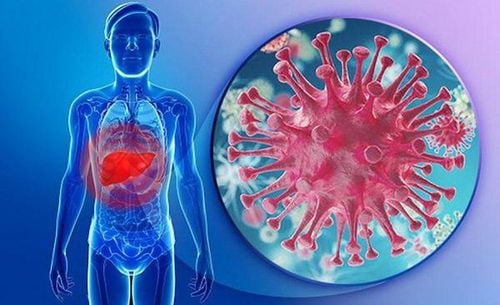
The liver is a relatively large internal organ located in the upper right corner of the abdomen. The role of the liver is to excrete digestive enzymes in bile, which is sent to the duodenum to break down the ingredients in food into smaller and easily absorbed nutrients. At the same time, the liver is also responsible for metabolizing and eliminating toxins in the blood from the body. Therefore, a healthy liver is an essential element to nurture children to grow up quickly.Acute liver failure in children occurs when many cells in the liver die or are severely damaged in a short period of time. This prevents the liver from working as it should. As a result, the patient may become lethargic, reduce alertness due to increased toxins in the blood, or even go into a coma.
Because the progression of acute liver failure in children is so rapid, early detection and prompt treatment of children are important, although the incidence of acute liver failure in children is rare.
2. What are the causes of acute liver failure in children?
Acute liver failure has many different causes.2.1. In infants
Infections: Herpes simplex, echovirus, adenovirus, hepatitis B, parvovirus Drugs or toxins: Acetaminophen is a common medicine used to relieve pain and reduce fever but can affect how the liver works. This can happen if a child is given the wrong dose of medicine or if too much is taken to bring down a fever in a short period of time; Cardiovascular diseases: cardiogenic shock, respiratory failure, myocarditis; Metabolic disorders: Galactose, tyrosin, iron stores, fatty acid oxidation; Immune dysfunction: Autoimmune hepatitis, immunodeficiency, congenital hemolytic syndrome.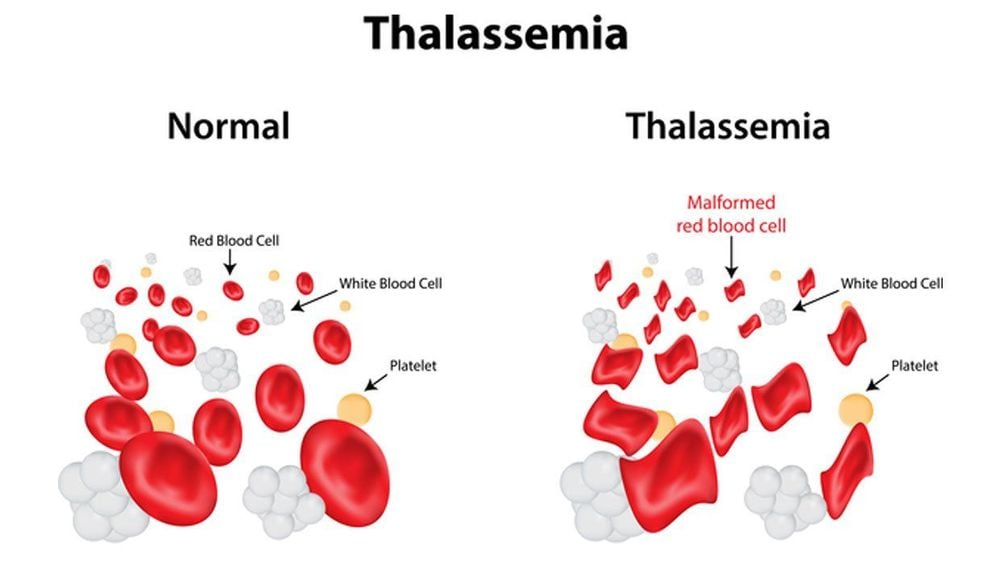
Tan máu bẩm sinh có thể là nguyên nhân gây suy gan cấp ở trẻ sơ sinh
2.2. In young children and older children
Infections: Hepatitis A, B and D, Epstein-Barr virus, cytomegalovirus, herpes, leptospirosis; Drugs or toxins: Valproic acid, isoniazid, halothane, acetaminophen, aspirin; Cardiovascular diseases: myocarditis, after cardiac surgery, cardiomyopathy, Budd-Chiari syndrome; Metabolic disorders: fatty acid oxidation, Reye's syndrome, leukemia; Immune dysfunction: autoimmune hepatitis, immunodeficiency, congenital hemolytic syndrome. However, there are some cases of children with acute liver failure but the cause cannot be found, this rate is about 44%. This number increases to 63% in children with acute liver failure under 2 years of age.3. What are the symptoms of children with acute liver failure?
Symptoms of acute liver failure in children may initially resemble those of a viral infection. This condition includes stomach pain, feeling constantly tired, poor appetite, and then rapidly progressing to jaundice, yellowing of the eyes, impaired consciousness, and blood clotting disorders.In hepatic encephalopathy, the awakening function of the brain is no longer working as it should. This happens when the liver is unable to metabolize or remove toxic products from the blood. Hepatic encephalopathy occurs when a child has sudden and severe liver failure. Newborns from birth to 28 days old may not have many obvious signs of hepatic encephalopathy, but can be detected by jaundice.
For infants from over 28 days old, the child has manifestations such as: irritability, crying a lot, constant irritability or maybe lethargy, wanting to sleep more during the day than at night.
Older children may always be angry, irritable, have trouble sleeping or feel sleepy all the time.
4. How to diagnose children with acute liver failure?
Laboratory tests and physical findings may indicate liver dysfunction. From there, the doctor will identify the child with acute liver failure based on:Signs of mental disorder due to hepatic encephalopathy; Jaundice ; Liver enzyme levels rise very rapidly and at a very high threshold; Clinical coagulation dysfunction with subclinical and cutaneous ecchymosis.
5. How to treat children with acute liver failure?
Treatment of acute liver failure in children is dependent on the underlying cause. Some causes can be treated with medication or a liver transplant.Supportive care. There are some children who will recover on their own with only symptomatic relief until liver function recovers. Often children with acute liver failure due to viral infection will have a better recovery rate. Treat the underlying disease. If your child has acute liver failure due to a cardiovascular condition or from taking acetaminophen, the condition can be treated with medication. However, if liver failure is due to metabolic disease, it may be somewhat reversible with appropriate medical therapy or dietary modification as soon as possible. Liver transplant. About 40% of children with acute liver failure require a liver transplant to survive. For most patients with no known cause of liver failure, organ transplantation is the only option. Whether a liver transplant is considered depends on: Whether the cause of the disease is known The likelihood that the transplant will be successful There is a systemic disease in more than one organ or part of the body Levels degree of brain injury Possibility of recovering brain sequelae after a liver transplant has operated. Treatment of brain diseases. Hepatic encephalopathy invariably progresses to hepatic coma with sudden and severe hepatic failure. Therefore, children need to be treated by trying to stop the production of more toxic products in the blood or remove them with a liver filter. Treatment of blood clotting disorders. Neutralizing drugs or blood products may be prescribed if the child's clotting function is not guaranteed until the liver recovers.

Trẻ em có thể được ghép gan để điều trị suy gan cấp
6. What is the prognosis of children with acute liver failure?
In general, acute liver failure in children is rare. The child's chance of recovery depends mainly on the cause and the age of the child. The stage of liver damage at detection and the extent to which brain parenchyma has been affected also have an impact on recovery. If the liver can heal on its own, most children will make a full recovery with no sequelae.The survival rate of children with acute liver failure if they receive a liver transplant is up to 90%. Most of these babies have a 70% survival rate after five years.
Although rare, acute liver failure in children is extremely dangerous due to its rapid progression and dysfunction of other organs, including the brain. Therefore, early detection, identification of causes and timely correction of liver function are extremely important for survival as well as long-term prognosis in children with acute liver failure.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.