This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Le Nguyen Hong Tram - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Nha Trang International General Hospital1. What is peritonitis?
Peritonitis is an infection of the peritoneum - the mesentery and peritoneum that surround the abdominal organs. The cause is usually bacterial infection and based on the mechanism of infection, peritonitis is classified as primary peritonitis or secondary peritonitis.
Whatever the cause, peritonitis is always a serious condition and is considered a surgical emergency. At this time, the diagnosis needs to be confirmed quickly in order to carry out active treatment steps, including surgery to localize the infection, avoid sepsis and save the patient's life.

2. Causes of peritonitis
2.1. Primary peritonitis Primary peritonitis is also called spontaneous bacterial peritonitis.
Patients with primary peritonitis have mostly vague gastrointestinal symptoms or sometimes no symptoms at all. The route of infection to primary peritonitis is hematogenous, lymphatic, or intraluminal transmission of bacteria through the intestinal wall. Patients with an underlying disease causing ascites, such as decompensated cirrhosis, which causes effusion in the peritoneal cavity, are at risk for primary peritonitis.
In clinical testing for primary peritonitis, approximately 90% of cases are culture positive for an agent. In particular, gram-negative bacteria are common pathogens such as Escherichia coli, Klebsiella pneumoniae, Bacteroides... while gram-positive bacteria such as Streptococcus pneumoniae are less common.
2.2. Secondary peritonitis Compared with primary peritonitis, secondary peritonitis is more common.
In most cases, this is an acute abdominal pain and is a complication of some extra-cavity pathologies occurring in the peritoneal cavity such as:
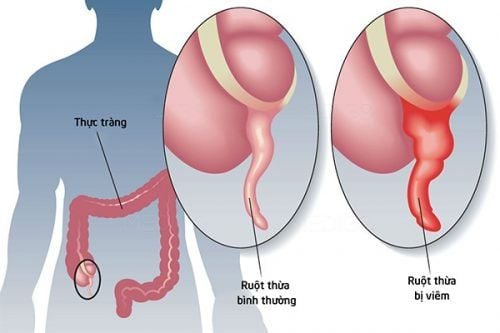
Perforation of hollow organs: gastric ulcer, diverticulitis, Necrotizing cholecystitis Inflammation of intra-abdominal organs: appendicitis, diverticulitis, necrotizing pancreatitis Post-operative complications: visceral infarction, perforated visceral trauma Intra-abdominal visceral biopsy Intra-abdominal trauma Abdominal visceral abscess ruptured and spread to the abdomen Because the source of infection in secondary peritonitis is quite diverse, culture specimens will give a positive result for mixed infection, including aerobic bacteria such as E. coli , Klebsiella, Enterobacter, Streptococci, Enterococci and also anaerobic bacteria such as Bacteroides, Eubacteria, Clostridia.
2.3. Other causes Peritonitis in immunosuppressed patients such as HIV/AIDS
Chemical peritonitis: inflammation of the peritoneum but not caused by bacteria, caused by irritating chemicals in the body such as blood, bile, urine or exogenous chemicals such as barium contrast when gastrointestinal tract is spread into the peritoneal cavity

3. What are the symptoms of peritonitis?
Signs and symptoms of peritonitis include:
Abdominal pain, which is the most common reason for hospitalization Bloating or abdominal discomfort Persistent smoldering fever Persistent high fever Nausea and vomiting Vomiting Loss of appetite Diarrhea Low urine output Thirst Diarrhea, defecation Fatigue, lethargy, or lethargy If peritonitis occurs in patients undergoing peritoneal dialysis, symptoms Peritonitis may also include cloudy dialysis, white streaks, fibers, or wisps in the dialysis fluid, and an unusual odor in the dialysis fluid or the area around the catheter site.
4. How is peritonitis diagnosed and treated?
Diagnosis of peritonitis is mainly based on physical manifestations. Analysis of peritoneal fluid is intended to confirm the diagnosis, while imaging studies can detect underlying conditions and rule out differential diagnoses when in doubt, especially when patients are hospitalized with symptoms of acute abdominal abnormalities due to metabolism in diabetic ketoacidosis or abdominal pain due to lead poisoning...
However, because this is an urgent condition, initiation of treatment should not be delayed until have test results. Accordingly, the core role in the treatment of peritonitis is to control the infection with antibiotics and the antibiotic regimen should depend on the classification of peritonitis:
4.1. Primary peritonitis Indicated for the treatment of primary peritonitis when the patient has a fever above 37.8°C, a polymorphonuclear leukocyte count in the ascites from more than 250 cells/μL and signs of perception change.
The antibiotic of choice is a 3rd generation cephalosporin broad-spectrum antibiotic such as cefotaxime, ceftriaxone.
4.2. Secondary peritonitis The approach to secondary peritonitis is to eliminate the source of infection with antibiotics and treat the underlying cause through interventional procedures when necessary. In addition, because the digestive system is severely damaged, the patient needs to be fasted and nutritional support through temporary parenteral nutrition and other supportive care measures.
Broad-spectrum antibiotic in secondary peritonitis is one of the following:
Piperacillin + tazobactam Ampicillin + sulbactam, possibly in combination with gentamicin Ciprofloxacin +/- metronidazole In severe peritonitis, use is indicated. carbapenems, such as imipenem or meropenem. In addition, the indication for surgery should also be established as soon as possible when the patient's condition allows. In this way, the surgeons can dissect, drain the infection, clean the abdomen, so that the infection can be controlled more thoroughly.

5. Complications and ways to prevent peritonitis
If not treated properly and aggressively in the first place, the infection in peritonitis can extend beyond the peritoneum, causing sepsis (bacteremia). This is an infection that spreads throughout the body with a very rapid progression, leading to shock and life-threatening. Because of this danger, prevention of peritonitis is extremely important. If peritonitis is associated with peritoneal dialysis, the entry is due to bacteria around the catheter. At this time, you need to take the following steps to prevent peritonitis:Wash your hands thoroughly with antibacterial soap under clean running water before performing peritoneal dialysis, paying attention to the skin under the nails Clean the area skin around the catheter with disinfectant every day Perform peritoneal dialysis in a hygienic, isolated area Wear a mask during the procedure Properly store the dialysis solution Do not keep pets indoors Frequently If you have had primary peritonitis before or if you have frequent accumulation of peritoneal fluid due to a chronic medical condition such as cirrhosis, consult your doctor. Doctors will prescribe long-term oral antibiotics to prevent future peritonitis. In summary, intra-abdominal infections are common in clinical practice and are the main cause of pathologies. Associated and fatal is peritonitis. Depending on the source of infection, peritonitis is divided into primary peritonitis and secondary peritonitis. Regardless of the causative agent, antibiotics should be indicated as soon as possible and surgical intervention should be considered when appropriate to actively save the patient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.