This is an automatically translated article.
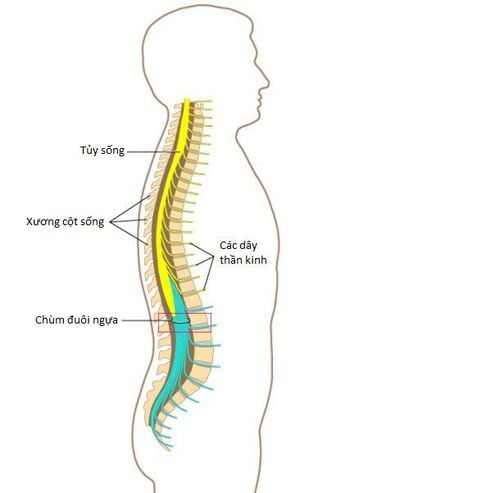
Possible complications of ventricular drainage surgery are quite common in patients with hydrocephalus. These factors will significantly affect the patient's health as well as quality of life. Accordingly, understanding the following information will contribute to knowing how to monitor and prevent disease risks for patients after ventricular drainage surgery in the long run.
1. Why does ventricular drainage surgery cause complications?
Ventricular drainage surgery is a very common neurosurgery and is often performed in specialized neurosurgery centers. However, the complication rate after ventricular drainage surgery is still remarkably high. Several epidemiological studies have shown that the failure rate after this intervention has been estimated at 11% to 25% during the first year after drainage. At the same time, the number of patients requiring a second intervention to repair the drain is still common, especially in pediatric patients than in adults.
The most common causes of complications after ventricular drainage in both children and adults are obstruction and infection. In which, the reason for infection is an early complication after ventricular drainage surgery and tubal occlusion is a late complication.
Despite significant advances in drainage improvements and valve design as well as aseptic techniques, the prevention of these complications has not demonstrated significant progress over several decades via. Thus, drain obstruction and infection remain common problems for clinicians to consider, and are reasons for hospitalization for repair and replacement. This not only reduces the patient's quality of life, but also costs the annual medical costs of each family and society.
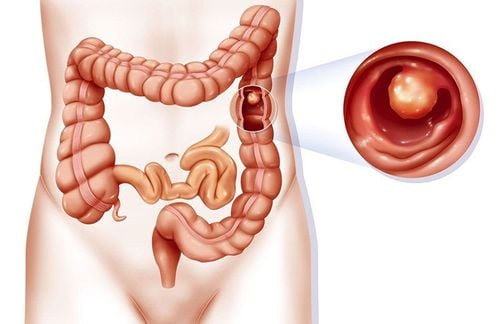
However, not only these two complications, ventricular drainage surgery also has other possible complications, including bowel perforation, pseudomembranous formation and excessive drainage... will be presented. detailed below.
Ngoài nhiễm trùng và tắc nghẽn ống dẫn, thì thủng ruột là một trong những biến chứng nguy hiểm của phẫu thuật dẫn lưu não thất
2. Possible complications of ventricular drainage surgery
2.1 Infectious complications after ventricular drainage surgery
Infection is a very common complication after ventricular drainage surgery with a reported incidence of about 8 to 15% among patients who have undergone the intervention.
The risk factor associated with infection after ventricular drain surgery is age (newborns are more susceptible to infections than young children and children are more susceptible than adults because the immune system is not fully developed. sufficient), CSF leak, indication for drainage is due to intraventricular hemorrhage and previous infection of the drain.
The majority of post-implantation CSF tube infections will occur within the first few weeks to months after insertion, although there are also cases of late infection with onset after the first year . At this time, the cause of early infection is often due to hygienic conditions and manipulation during the intervention; In contrast, the causes of late infection were due to cases of peritonitis, pseudomembranous peritoneum, intestinal perforation and intravenous drug use.
Therefore, in clinical practice, if a patient has symptoms of an ineffective drain, such as nausea, vomiting, headache, and is accompanied by fever, an infectious factor should be suspected first. . This is considered a serious complication with a high rate of need for re-intervention as well as a high risk of death if not conducted promptly.
The most common pathogens isolated from infected CSF drains in order of frequency were Staph cholermidis, Staph aureus, gram-negative bacteria. In which, most of these agents are common skin flora and infection will often occur during tube insertion due to contamination from the skin.
At this point, the standard treatment for an infectious complication is removal of the drain in conjunction with intravenous antibiotics, and the inpatient stay is certainly a lengthy, weekly process. to the hospital every month. During this time, the patient will have an alternate external drain placed until the infection clears and another tube is implanted at a safer time.
Therefore, efforts to develop means to prevent infectious complications after ventricular drainage surgery are of paramount importance to help reduce treatment costs and reduce morbidity. Some solutions that have been applied are using antibiotic-impregnated catheters, using prophylactic antibiotics before surgery, optimizing aseptic technique as well as reducing intervention time to a minimum.
2.2 Complications of drainage duct obstruction after ventricular drainage surgery
Drainage obstruction after ventricular drainage surgery is by far the most common cause of postoperative failure. However, the factors contributing to this problem are still not clearly understood.
Obstruction can occur in the proximal catheter, in the valve or in the distal catheter. However, the most common site of obstruction in most studies was at the proximal catheter. Neurosurgeons have speculated that the proximal catheter may become blocked from within the brain parenchyma as it is inserted through the dura mater into the ventricles. Even so, protecting the catheter with a removable sheath when inserted through the cortex did not reduce the rate of need for later repair intervention.
Some other theories suggest that the proximal catheter may become obstructed with choroidal plexus tissue or debris, such as blood and proteins, which may gradually accumulate within and eventually block the catheter. Therefore, in practice, when a patient presents with symptoms of drainage obstruction such as headache, lethargy, nausea, and vomiting, a diagnosis of this complication should be made and promptly confirmed by cranial computed tomography. Brain. After that, corrective intervention should be promptly planned, especially when the patient has signs of suspected infection.
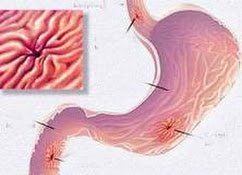
2.3 Complications of intra-abdominal pseudomembranous cysts after ventricular drainage surgery
Formation of intra-abdominal pseudomembranous cysts is a rare complication after ventricular drainage compared with the two obstructive and infectious complications mentioned above. The frequency with which this complication has been reported in interventional patients ranges from 1 to 4.5%.
Pseudocyst development usually occurs in the late stages with most cases occurring a year or more from the time of initial intervention as well as after subsequent repairs. The cyst is essentially a collection of fluid that accumulates around the distal catheter tip and is surrounded by a "wall" of pseudomembranous tissue. The formation of these pseudomembranous tissues is thought to result from inflammation and adhesions of the peritoneum. This can occur with complications of infection of the drain or after surgery or interventional procedures in the abdomen.
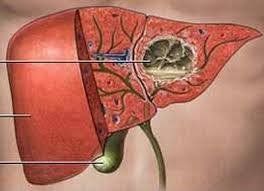
The most common presentation of patients with intra-abdominal pseudomembranous cyst complications after ventricular drain placement is abdominal pain and distention, sometimes with a palpable intra-abdominal mass. Different from the above two complications, neurological symptoms are sometimes not noted. Even, some rarer cases of pseudomembranous cysts in the abdomen are liver cysts. This can occur when the distal catheter moves to the surface of the liver and causes chronic irritant inflammation. At this time, patients often present to the doctor because of right upper quadrant abdominal pain, which increases after meals, and may be accompanied by elevated liver enzymes.
At this point, the diagnosis is best made with ultrasound or abdominal computed tomography, both to identify complications related to the drain, and to rule out other local conditions with similar symptoms. copper. Once the diagnosis is made, the decision to treat will depend on whether the drain is infected and the effects that an intra-abdominal pseudocyst can cause and the goals of prevention. Occur again periodically.

Một trong những biến chứng nguy hiểm sau phẫu thuật dẫn lưu não thất là nang giả mạc
2.4 Complications of intestinal perforation after ventricular drainage surgery
Catheter perforation after ventricular drainage surgery is a rare complication. The estimated incidence of this event is between 0.1 and 0.7%.
The most commonly reported cause is stiffness of the distal catheter tip over a prolonged period of time on the intestinal wall. Although some cases have been reported in adults, the majority of bowel perforations due to distal catheters have occurred in children. This may be because children have relatively thin, vulnerable intestinal walls, especially in infants. At this time, the friction force will increase the influence of the catheter on the intestinal wall and ultimately cause intestinal perforation.
2.5 Complications of thrombosis and subdural hematoma after ventricular drainage surgery
The formation and growth of thrombus and excessive subdural hematoma following ventricular drainage surgery can become complications of this type of intervention. Some have reported the incidence of thrombosis and subdural hematoma after drainage as being approximately 5% in patients requiring intervention as indicated by high-pressure hydrocephalus.
The treatment of this complication will depend on its progression. If the thrombus and subdural hematoma resolve spontaneously, it is considered benign and does not require intervention. In contrast, others can rapidly grow, causing a significant mass effect and manifesting as neurological symptoms. At this time, the repair intervention is a mandatory indication, not only to help preserve the patient's life but also to ensure the function of the remaining brain parenchyma.
In summary, the possible complications of ventricular drainage surgery are difficult to completely avoid, often leading to prolonged hospital stay as well as heavier treatment costs. Despite many advances in interventional techniques, patients with drained hydrocephalus still often need to have their ducts repaired several times throughout their lives. Accordingly, to prevent related complications, patients need to be detected early and corrected promptly, limiting further sequelae in the long term.
References: moh.gov; vnha.org.vn
MORE:
Treatment of ventricular dilatation in children Symptoms and treatment of acute epidural hematoma Neonatal purulent meningitis: Diagnostic tests