This is an automatically translated article.
Compared with medication, placing deep brain electrodes for Parkinson's patients is a treatment method with better results. With the cost of treatment only 1/3 of foreign countries, placing deep brain electrodes will be more widely applied to patients.
1. What is Parkinson's disease?
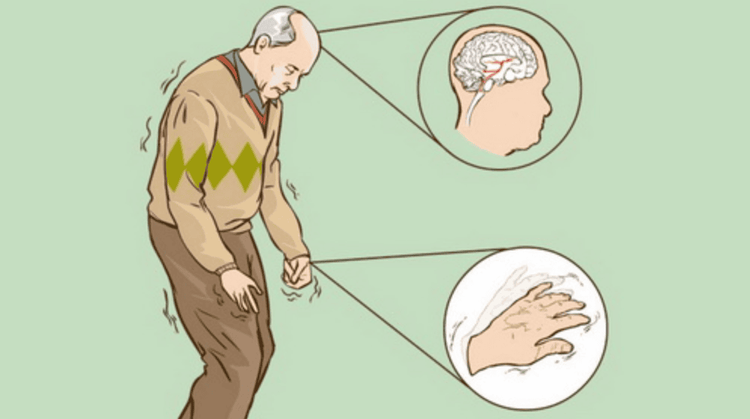
Parkinson's disease is known to be a common disease in the elderly. The disease is the degeneration of dopaminergic neurons, which progresses gradually and becomes more severe over time.
The most common symptoms that we often see in Parkinson's patients are foot tremors, slow hand tremors, postural instability, so it is easy to fall.
When the disease is more severe, the patient will not be able to control simple movements such as dressing, holding chopsticks, bowls, nocturia, constipation,...
When the disease is detected, the patient mainly uses it. medication to limit tremors of the extremities. Usually medications are effective during the early stages of the disease. But later on, the drug is no longer effective for the patient, the doctor will prescribe an increase in the dose and this stage appears more complications.
At this point, there is a need for another treatment to replace the drug and bring more effective.
Bệnh Parkinson ở giai đoạn nặng sẽ bị run các đầu chi và không tỉnh táo
2. Deep brain stimulation by placing electrodes
Deep brain stimulation aims to insert electrodes into deep brain sites. This method is indicated for the treatment of Parkinson's disease and diseases related to movement disorders. This is a modern and advanced technical method that is very popularly applied in countries with leading medical development such as Europe and the US.
Deep brain stimulation surgery with electrode placement is understood as inserting a metal rod (also called an electrode) into the correct structures deep in the brain. This electrode is connected to a wire leading out of the brain, threaded under the skin from the head area to the front of the chest, and then attached to a pacemaker placed there.
Depending on the high or low power usage, the battery has a long life, but the average is about 5 years. The electric current will follow the wire to the electrode, thereby affecting the brain nucleus to help improve symptoms for the patient.
However, this method is not indicated for patients with dementia, cognitive disorders, psychosis.

Kích thích não sâu bằng cách đặt điện cực giúp cải thiện triệu chứng cho người bệnh.
3. Conducting deep brain electrode placement
Step 1: Prepare
On the hospital side:
The surgery needs a team of highly skilled and experienced doctors and nurses. Includes: One main surgeon, one auxiliary surgeon; 1 neurologist and 1 technician adjusts the current recorder; 2 nurses; 1 doctor and 1 anesthesiologist. Instruments are fully prepared including: Equipment to conduct endotracheal intubation; Specialized craniotomy kits for Parkinson's; Positioning frame (Stereotaxy); Deep electrodes, electrical excitation pulse generators; C-Arm camera; Consumables,... On the patient's side: Clean hair, clean surgical area. At the same time, the patient is clinically examined with magnetic resonance imaging, tests for surgery, indications for surgery and, especially, a written commitment to surgery. Step 2: Carry out surgery
At the first surgery:
The patient's head will be attached to a three-dimensional positioning frame (Stereotaxy) to guide the electrodes into the brain. Diagnostic imaging by magnetic resonance imaging and brain CT scan. In order to determine the exact location of the nucleus accumbens causing the symptoms of Parkinson's disease, it is necessary to program the electrode placement. Patients are placed deep brain electrodes in the operating room under anesthesia. The drilling site is just anterior to the fronto-parietal joint, about 2.5 cm from the midline, about 1 cm in diameter. Can be 1 side or 2 sides. Through computer calculations and checked by intraoperative C-arm, the recording electrode is inserted into the brain at a depth and angle. The test will be performed at the diseased brain nucleus with a very low intensity electric current and monitor the actual effectiveness of the patient during surgery. The neurologist will determine the intensity of the stimulation current based on the anti-vibration effect, affecting the ability to read and see. Place the stimulation electrode: when all the parameters have been determined, the electrode is fixed to the patient's position and the intensity parameter is adjusted accordingly through the channels. The electrode is placed under the scalp in the occipital region, and the tip is poked out through the skin. The internist will evaluate the effectiveness of stimulators with different intensities and clinical effects over a period of a few days to a week. After 1 week from the first surgery, there will be the second surgery:
Implant the IPG stimulator under the skin of the chest and below the clavicle. The patient is under general anesthesia. Subclavian skin incision on the same side with deep brain electrode. Create a tunnel under the skin from behind the ear to below the collarbone, and the wire from under the scalp to below the collarbone, connecting the wire to the electrode implanted in the brain. Place the IPG stimulator under the lever, connected to the power lead. Finally set up the operation program of the IPG. The entire device works thanks to a battery placed under the skin of the chest area. Average battery life is 5 years depending on high or low power usage.

Trước khi tiến hành đặt điện cực não sâu, người bệnh cần chụp MRI
4. Post-surgery
Patients need to be closely monitored after surgery such as: Incisional bleeding, mental status, seizures After the first surgery: the neurologist will detect the most appropriate amperage for the patient first. at the second surgery, put a permanent IPG electric stimulator. Exercise physical therapy in place and walking. Some complications may occur with patients with deep brain electrode placement: Bleeding; infection; language disorder ; epileptic ...
If bleeding case needs tomography scan to evaluate and treat Patient has postoperative infection depending on the severity to treat with drugs or remove electrodes If the case occurs Epilepsy requires CT scans to find the cause and can be treated with antiepileptic drugs. Any questions that need to be answered by a specialist doctor as well as customers wishing to be examined and treated at Vinmec International General Hospital, please book an appointment on the website to be served.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.