This is an automatically translated article.
When the nerves or motor nerves that control the movement of the limbs in the body are damaged, the patient will experience problems with movement disorders. In this case, the doctor will conduct a physical exam for the patient to assess the disorder as well as come up with the most effective treatment plan for the patient.
1. What is a physical exam?
Movement disorder with the main cause of motor nerve damage makes the patient unable to control part or all of the body and causes difficulties in daily activities.
The following are some of the most common movement disorders:
Ataxia; Parkinson disease ; Tourette's syndrome; Spastic paralysis; Essential tremor; Muscular dystonia; Huntington's disease. To assess the degree of movement disorder caused by damage to the motor nerves in the whole body or a part of the patient's body, the specialist doctor will appoint the patient to perform a motor examination to evaluate. Determine the strength of the patient's upper and lower limbs, thereby giving the most appropriate course of treatment for the patient.
Mobility examination is done through observing the patient's movement status and through a few specified movements to assess muscle tone, strength, posture and motor coordination of the patient.

Bệnh Parkinson là một dạng rối loạn vận động thường gặp
2. How is the physical examination conducted?
2.1 Observe the patient's upper and lower extremities The doctor will observe and evaluate the following problems:
Observe the patient's muscles, assess the patient's muscle condition to see if they are in good condition. normal or not, muscle atrophy or hypertrophy or not. When the patient is at rest, the muscle bundles may experience small and mild tremors without displacement of the joint for a variety of reasons.
The patient's resting activities may be hyperactivity due to restlessness or restless legs or hypoactivity common in patients with depression, Parkinson's disease, patients with midfrontal gyrus dysfunction. There are also spontaneous movements such as tremor, chorea, dystonia.
2.2 Physical exam The purpose of performing a physical exam is to evaluate or detect increased muscle tone or decreased muscle tone in the patient.
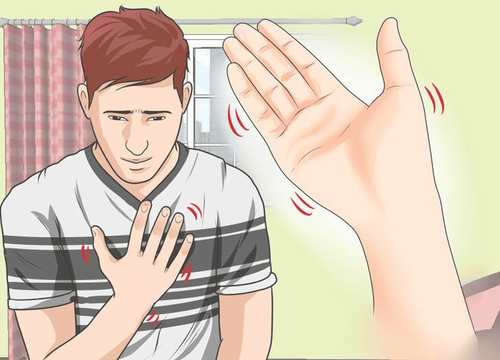
The patient is asked to lie down and relax the limbs, the doctor will conduct a patency test by gently squeezing the muscles in the forearm, arm, thigh and leg. In addition, to evaluate the contractility by passively moving and flexing the limb at the elbow, wrist, and knee joints. Assess the degree of flapping by gently shaking the patient's forearm and lower leg. Through the physical exam, the doctor will assess the patient's condition, if the patient has characteristics such as strong muscles, when the patient is convulsive, has very little resistance to passive movements and gently wagging hands and feet, these are signs of a normal person.
Khám cơ lực giúp đánh giá hoặc phát hiện tăng trương lực cơ hoặc giảm cơ lực cơ ở người bệnh.
In cases where increased muscle tone will cause muscle stiffness because increased resistance in both the flexor and extensor groups produces lead-tube stiffness. There are also cases of cogwheel muscle stiffness, pyramidal rigidity...
Cases of decreased muscle tone due to cerebellar disorders, neuromuscular disorders. In neonates, hypotonia is mainly due to neuromuscular or central nervous system disorders.
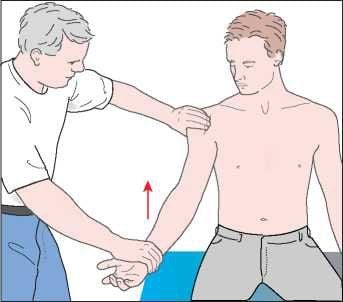
2.3 Muscle strength The doctor informs the patient about the physical examination, at this time the patient can sit or lie on the hospital bed depending on the doctor's request. During the examination, the doctor will assign the patient to perform the following movements:
For upper limb muscle strength To form and close the arm, bring the arm forward and backward with zero and resistance of the examiner. Flexion and extension, pronation and supine forearm with air and with examiner resistance.
Flexion and extension of the hand with no and with examiner resistance.
Extension and closure, flexion and extension of fingers with zero and resistance by examiner

Khám sức cơ chi trên bằng cách gập, duỗi bàn tay
For lower limb muscle strength, add and lift the thigh with zero and with examiner resistance.
Bend and extend the leg with no and with examiner resistance.
Flexion and extension of the foot with no and with examiner resistance.
Extend and flex the toes with no and with examiner resistance.
Scale for assessing muscle strength in motor examination:
Grade 0/5: Total paralysis. Grade 1/5: Visible muscle movement, but no joint movement. Grade 2/5: Joint movement, but no gravity. Level 3/5: Overcoming gravity, but not resistance. Grade 4/5: Resistance to resistance, but not reaching normal muscle strength. Grade 5/5: Normal muscle strength 2.4 Patient's posture Abnormalities of the patient's posture may be due to defects in some central or motor nerves. To examine movement, the doctor will perform a number of tests as follows:
Romberg test: Ask the patient to stand up straight, put his feet together, open his eyes, then close his eyes. Patients may stand upright with eyes open, and stagger (to fall) with eyes closed due to disturbances in either depth perception or vestibular function because vision can compensate for both. Visual acuity cannot compensate well for cerebellar ataxia, so this patient staggers even with his eyes open. Patients with cerebellar ataxia also stagger when their eyes are closed, but are not called Romberg positive

Romberg test giúp xác định dáng điệu bất thường của người bệnh
Pull test: The examiner stands with his back to the wall so he can lean on it when needed. Ask the patient to stand upright with his back to the examiner, 30-60cm away, feet together, eyes open. Pull the patient's shoulder firmly and quickly back toward the examiner. Check for postural loss if posture may be affected in neuromuscular or basal ganglia disorders. Seen in Parkinson's syndrome, patients have lesions on the forehead or bilateral white matter. Have the patient balance, walk freely, or walk normally in a straight line to assess the patient's balance, stride length and regularity, rotation, and movements. attached arm. Note that if the patient cannot walk steadily, make sure someone is accompanied to support the patient, to avoid the patient falling. 2.5 Coordination of movement The doctor assigns the patient to perform some movements as follows:
Finger pointing: Ask the patient to touch the examiner's nose with their index finger and then touch the patient's nose. Repeat the above movement several times until you can see that the movements are smooth and precise. Heels, knees: The patient is in the supine position. Ask the patient to lift one leg, then place the heel on the knee of the other leg and slide the heel steadily down along the crest of the tibia to the instep. Patients with cerebellar hemispheric disease will move (finger or heel) irregularly but jerkily in steps, possibly off target (disturbance).

Ngón tay chỉ mũi là một trong những bài kiểm tra vận động thường dùng
Rapid movement movements: Ask the patient to alternately pat the palm of one hand with the palm and back of the other hand at regular intervals, as quickly as possible. You can clap 3 times with the palm of your hand, then change to clapping with the back of your hand 1 time, and so on, repeat as quickly as possible. Patients with ataxia will not be able to maintain rhythmic variations in amplitude and movement speed will be irregular. The average person will stop the hand quickly and the hand will be returned to the original position without going too far. Reflection: Ask the patient to stand or sit, straighten the arms, legs, and hands in front, palms down, eyes closed. Hit the forearm firmly with your hand to push the arm down. Patients with cerebellar disease will not be able to control the movement down quickly, then lift back too far, so that the arm will "bounce" higher than the original position. Mirror movements: Put the index finger of another's hand in front of the patient, 30-60cm away from the patient. Ask the patient to also bring the index finger close but not to touch. Then quickly move the examiner's finger to a new position 30cm away from the old position. Repeat several times to assess patient mobility. Patients with cerebellar dysfunction will go too far from the target and each move must be adjusted one or more times to get close to the target. Movement disorders, if not detected early and treated promptly, will cause long-term damage to the brain, affect quality of life and cause many serious complications. As soon as abnormal symptoms appear in movement, you should immediately go to a reputable medical facility for an exercise examination.

Khám vận động giúp phát hiện ra rối loạn vận động sớm tránh tổn thương lâu dài đến não
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
For detailed information on how to register for examination and treatment, please contact Vinmec Health System nationwide.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.