This is an automatically translated article.
The article was professionally consulted with Master, Doctor Nguyen Minh Son - Interventional Cardiologist - Department of Medical Examination & Internal Medicine - Vinmec Nha Trang International General Hospital.Diuretic peptide test is also one of the important tests that play a significant role in diagnosis and treatment monitoring. Let's find out what Peptide diuretic is and the role of this test in diagnosing heart disease in the article below.
1. What is a diuretic peptide?
The percentage of patients with heart failure is increasing with age. In the age group from 45 to 54, this percentage accounts for 1-2%, and 10% of the population is over 75 years old. Therefore, biological tests today are very important in diagnosis and prognosis as well as monitoring the effectiveness of treatment.Diuretic peptide (BNP) is a protein secreted by the ventricular muscle in response to volume or pressure overload. Since its discovery more than 30 years ago, BNP has emerged as an important biomarker in the diagnosis of congestive heart failure (CHF). It is valuable in assisting the diagnosis of congestive heart failure and predicting long-term mortality. Its use has also been explored in ischemic heart disease, myocardial infarction, and in acute pulmonary embolism (PE).
2. Mechanism of action of Peptide Diuretic
Type B Sodium Diuretic Peptide (BNP) is a member of the family of four human sodium diuretic peptides that share the same 17-peptide ring structure. The first substance was identified in 1983 and named atrial sodium peptide (ANP). ANP is a 28-amino acid polypeptide derived from the C-terminus of the prohormone proANP. The primary source is located in the atria of the heart, and ANP is rapidly secreted in response to atrial contraction. The normal heart secretes very small amounts of ANP, but elevated levels are found in patients with left ventricular hypertrophy (LV) and mitral valve disease.However, the diuretic peptide was later found to be present in high concentrations in cardiac tissues, especially the ventricles. Two peptides, the C-type sodium diuretic peptide (CNP) and the Dendroaspis sodium diuretic peptide (DNP), have also been described; they are thought to act in the peripheral and atrial vasculature, respectively.
Prior to activation, the diuretic peptide is stored as a 108-amino acid polypeptide precursor, proBNP, in secretory granules in both the ventricles and to a lesser extent in the atria. After proBNP is secreted in response to mass overload and consequent myocardial stress, it is cleaved to 76-peptide, bioinert N-terminal NT-proBNP and 32-peptide, bioactive diuretic peptide hormone. These two fragments are secreted into plasma in equal amounts and both have been clinically evaluated for use in the treatment of congestive heart failure (CHF).
High ventricular filling pressure stimulates ANP and BNP release. Both peptides have diuretic, sodium-diuretic, and antihypertensive effects, acting by inhibiting the renin-angiotensin-aldosterone system. They also have systemic and renal sympathetic activity. In addition, peptide diuretics may provide a protective effect against the remodeling and fibrosis that are harmful as heart failure progresses.
Although ANP was identified first, the concentration of BNP in myocardial tissue was later found to be higher than that of ANP. Therefore, BNP has been studied more strongly than ANP as a clinically useful marker of increased ventricular filling pressure. Elevated levels of diuretic peptides are indicative of increased left ventricular (LV) filling pressure and LV dysfunction.
Diuretic peptide receptors and plasma endopeptidases actively clear diuretic peptides from the circulation; The plasma half-life is very short, about 20 minutes. No receptor-mediated clearance of NT-proBNP is known to occur, and NT-proBNP has a prolonged half-life of 60-120 minutes, respectively. As a result, plasma NT-proBNP concentrations tend to be 3-5 times higher than BNP concentrations. Clearance of NT-proBNP is thought to be primarily renal. Therefore, the renal clearance of NT-proBNP confounds its diagnostic utility in patients with renal impairment.
As a laboratory specimen, NT-proBNP is more stable during storage than a diuretic peptide. The NT-proBNP sample was stable at room temperature for 72 h, in contrast to the diuretic peptide sample which was less than 4 h.
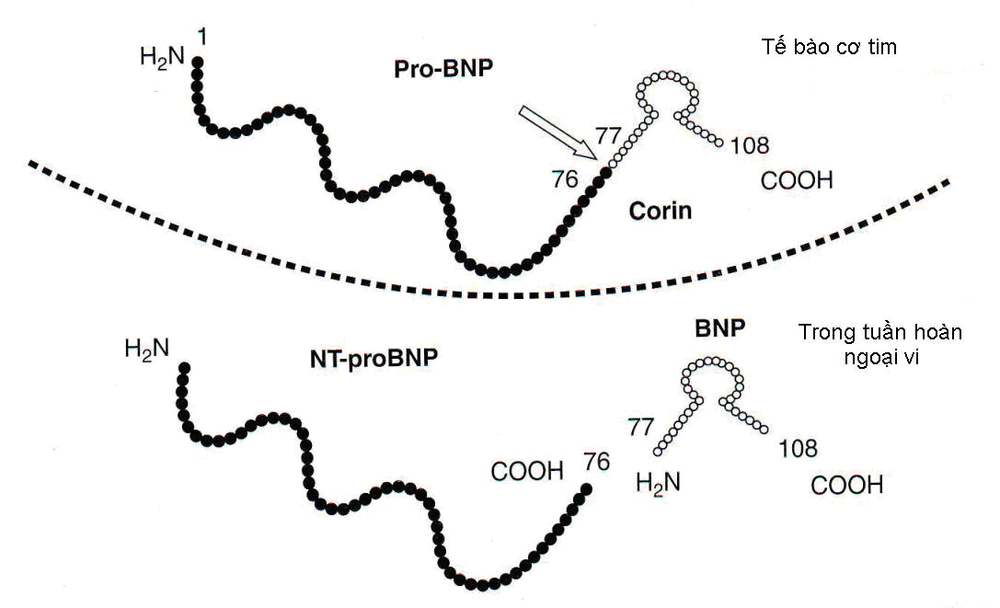
Peptide lợi niệu và Pro BNP được tổng hợp trong tế bào cơ tim, sau đó chia làm 2 phân tử đi vào máu ( NT-proBNP và BNP )
3. Peptide diuretic in the treatment of heart disease
3.1. Diuretic Peptides in the Emergency Department Level B diuretic sodium peptide (BNP) is a more accurate predictor of heart failure than history, physical examination, and routine laboratory tests. The trial showed that a diuretic peptide level ≤100 pg/mL confers 90% sensitivity and 76% specificity in separating the heart from noncardiac causes of dyspnea. NT-proBNP has also been studied in the emergency room (ED), during hospitalization, and even in the outpatient setting, to help diagnose, determine disease severity, confirm its use as a good biomarker for cardiovascular risk assessment.3.2. Diuretic peptides in risk stratification Diuretic peptide measurements are a useful tool for risk stratification; in fact, high levels are associated with readmissions and risk of sudden death. Several studies have shown that diuretic peptide levels are the strongest predictor of subsequent mortality or hospitalization within 6 months. In the Australia-New Zealand Heart Failure Group Trial in patients with chronic heart failure and reduced systolic function, higher than average levels of NT-proBNP were associated with an increased risk of new decompensated heart failure events and death. all-cause mortality during 18 months of follow-up. The largest study, the Valsartan Heart Failure (Val-HeFT) trial in patients with chronic heart failure, found that: a 500 ng/L increase in baseline NT-proBNP levels increased the risk of death by 3, 8% and 3.0% with hospitalization for heart failure. On a multivariate analysis, NT-proBNP again ranked as the first prognostic factor in these patients, independent and stronger than traditional risk factors, such as left ventricular dilatation or dysfunction renal dysfunction.
3.3. Cardiovascular effects of peptides Diuretic peptide tests are also associated with several indices of systolic and diastolic function. Recently, it has been shown that diuretic peptides are involved in aggravation of systolic heart failure, degree of diastolic dysfunction, severity of mitral regurgitation, and RV dysfunction. Diuretic peptides also reflect elevated left ventricular filling pressure and pulmonary capillary pressure when measured invasively with good accuracy and specificity. In contrast, sensitivity is usually modest, particularly in patients with preserved systolic function and normal LV volumes. The best correlation between diuretic peptides and invasive measurements was demonstrated with end-diastolic ventricular wall tension and end-diastolic pressure.

Ứng dụng xét nghiệm Peptide lợi niệu trong điều trị bệnh tim
4. Application of quantitative plasma diuretic peptide concentration in clinical practice
4.1. Applications in diagnostics. Quantification of plasma diuretic peptides helps to confirm the diagnosis of heart failure, especially when the patient has clinical symptoms (fatigue, dyspnea, chest heaviness, little urine output, third heart sound, distended neck veins, rales stagnation in the lungs, peripheral edema), changes in the electrocardiogram, enlarged heart shadows on radiographs, decreased left ventricular ejection fraction on echocardiography.Quantification of plasma diuretic peptides also helps diagnose diastolic heart failure. Plasma BNP concentrations are increased in left ventricular hypertrophy, cardiomegaly, atrial fibrillation, myocardial infarction, and acute coronary syndromes.
In the case of patients with dyspnea, plasma diuresis peptide quantification allows the distinction between dyspnea due to heart failure (high diuretic peptide) or dyspnoea due to bronchopulmonary disease (normal diuretic peptide).
There is a correlation between the increased plasma concentration of diuretic peptides and the severity of heart failure according to the NYHA (New York Heart Association) classification in clinical practice. The increase in plasma diuretic peptide is inversely related to left ventricular ejection fraction (inverse correlation) and is directly related to myocardial volume and pulmonary artery pressure.
4.2. Treatment monitoring Quantification of plasma diuretic peptides allows for optimal treatment of heart failure (plasma levels of BNP decrease as clinical symptoms of heart failure subside, left ventricular ejection fraction improves and decreased pulmonary artery pressure). In general, diuretics, nitrate derivatives, aldactone, ACE inhibitors and receptor blockers, and beta-blockers are capable of reducing plasma diuretic peptide concentrations (with the exception of digoxin). In contrast, in hypertensive patients, beta-blockers are likely to increase the concentration of diuretic peptides.
4.3. Prognosis: Plasma diuretic peptide levels have prognostic significance in patients with heart failure and after myocardial infarction.

Nồng độ peptide lợi niệu có vai trò quan trọng trong tiên lượng điều trị bệnh tim
5. Factors affecting the diuretic peptide/NT-proBNP . test
The concentration of diuretic peptide and NT-proBNP increased in the presence of renal failure, the concentration of NT-proBNP was higher than that of diuretic peptide. NT-proBNP levels may be elevated simply on the basis of a normal age-related decline in estimated glomerular filtration rate (GFR). When GFR is less than 60 mL/min, NT-proBNP levels can be very high and their value in diagnosing heart failure in this setting is unclear. For peptide diuretics, an increase in the exclusion threshold of 200 pg/mL is recommended when the GFR is less than 60 mL/min.Natriuretic peptide levels may be moderately elevated in chronic lung disease when right ventricular overload occurs. NT-proBNP and diuretic peptide levels may also be elevated in acute pulmonary embolism. Although elevated levels are not diagnostic for pulmonary embolism, high levels may predict a worse prognosis, especially when noted together with elevated troponin levels. In about 20% of patients with lung disease, the concentration of diuretic sodium peptide is elevated. The increase in this setting may be due to heart failure, combined heart failure and pulmonary disease, arrhythmia or acute pulmonary embolism.
Patients with a body mass index (BMI) greater than 30 kg/m 2 have low levels of diuretic peptides and NT-proBNP. The diagnosis of heart failure must then be carefully considered in the appropriate setting, even if the levels are below the cut-off point.
Natural peptides are independent predictors of mortality in heart failure. Elevated or persistent levels of diuretic sodium peptide despite treatment suggest disease progression or treatment resistance. In the acute phase, a non-reducing diuretic peptide or NT-proBNP level with treatment is a poor prognostic factor that may require increased treatment.
Daily Natriuretic peptide levels should not be measured. It is recommended to measure levels at admission, after 24 hours of treatment, and at discharge. Decreased diuretic sodium peptide levels predict good outcome
Screening for diuretic peptides or NT-proBNP is generally not appropriate for asymptomatic, low-risk patients. Screening may have some value in populations with certain risk factors (eg, previous myocardial infarction, diabetes mellitus, uncontrolled long-term hypertension); however, echocardiography may remain the study of choice to evaluate left ventricular function.
ACCF/AHA Recommendations The ACCF/AHA makes a Class I recommendation for the use of diuretic peptide or NT-proBNP values in the diagnosis of heart failure in patients on emergency mechanical ventilation, especially when the diagnosis is not certainly, as well as their use in establishing prognosis or disease severity in the emergency department of patients with chronic heart failure. The indications recommend class IIa for the use of diuretic peptides or NT-proBNP to determine optimal dosing for selected clinically selected emergency patients who are hypovolemic and on medical treatment. in a heart failure management program.
For hospitalized or emergency patients, the ACCF/AHA makes a Class I recommendation for the use of a diuretic peptide or NT-proBNP in the diagnosis of acute decompensated heart failure, particularly when the diagnosis is uncertain, as well as as the use of diuretic peptides or NT-proBNP and/or cardiac troponin in establishing the prognosis or severity of acute decompensated heart failure in these patients. However, guidelines indicate that the usefulness of diuretic peptides or NT-proBNP in guiding treatment in hospitalized or emergency patients with acute decompensated heart failure remains unconfirmed.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













