This is an automatically translated article.
The article was professionally consulted with Master, Doctor Cao Thanh Tam - Cardiologist - Cardiovascular Center - Vinmec Central Park International General Hospital.Ventricular septal defect and atrial septal defect are common congenital heart diseases. If not treated early, these diseases can lead to many dangerous, life-threatening complications. Currently, the most commonly used treatment method for these two diseases is occlusion of the ventricular septal defect and atrial septal defect.
1. Learn the technique of occlusion of the ventricular and atrial septal defect
Ventricular septal defect is a common congenital heart disease, accounting for about 20% of congenital heart diseases. Long-term complications of the disease include: pulmonary hypertension, infective endocarditis, right heart failure or total heart failure. For treatment, the doctor appoints a technique to close the ventricular septal defect with an instrument to repair this defect, helping the physiology of blood flow in the heart return to normal. This is the technique of sealing the ventricular septal defect.Atrial septal defect is a common congenital heart disease. Among the types of atrial septal defect, atrial septal defect is the most common. The main treatment is occlusion of the atrial septal defect in cases of secondary septal defect, which allows for thorough treatment without surgery.
Currently, occlusion of the ventricular and atrial septal defect is an effective and safe method of congenital heart disease.
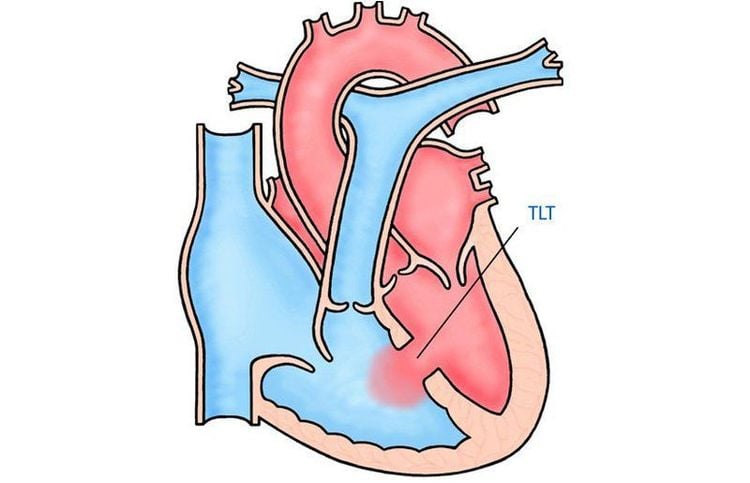
2. The technique of sealing the ventricular septal defect
2.1 Indications Pericardial ventricular septal defect or ventricular septal defect; Patients with a history of infective endocarditis; Ventricular septal defect affects hemodynamics; There is a ventricular septal defect with significant left-right shunt, left ventricular dilatation, increased left ventricular end-diastolic diameter relative to body area and age; Not accompanied by other lesions requiring surgery with extracorporeal circulation such as mitral regurgitation, aortic regurgitation, subaortic stenosis; If it is a ventricular septal defect, the septal defect is not larger than 10mm, the aortic ridge is more than 3mm, without too large aneurysms. 2.2 Contraindications Pregnant women; People with blood clotting disorders, bleeding; Echocardiography or cardiac Doppler detects the presence of warts in the heart chambers, blood vessels or shunt through the ventricular septal defect, which is a right - left shunt; Having a serious illness or other acute illness; The patient is allergic to the contrast medium; Children weighing less than 5kg; People with serious abnormalities of the thoracic or spine anatomy; The patient did not consent to occlusion of the ventricular septal defect with an instrument; In the case of patients with too high pulmonary artery pressure, occlusion is contraindicated if pulmonary resistance exceeds 7 Wood units or Rp/Rs > 0.5. 2.3 Preparation for implementation Personnel: 2 doctors and 2 technicians specializing in interventional cardiology; Equipment: Instrument table, sterile gauze, pump of all sizes, 3-prong device, arterial and venous access kit, catheters, ventricular occlusion device, instrument delivery system , Guidewire (conductor),...; Patient: Explained about the procedure, agreed to do the procedure, signed the written commitment; the patient is a child who needs endotracheal anesthesia, so it is necessary to prepare as carefully as before surgery; patients over 12 years old can perform the procedure under local anesthesia; Young patients need to induce sleep in combination with the use of pain relievers during the procedure; Medical records: Prepare complete records as prescribed.
2.5 Common complications and how to manage Air embolism or thrombosis: The doctor needs to expel gas, pay attention to anticoagulation for the patient; Pericardial effusion due to tear, perforation of the atrioventricular, ventricular, ... related to technical manipulation needs to be detected, drained early and may need early surgery; Hemolysis: A rare complication, usually due to residual shunts. The treatment in this case is to closely monitor and give adequate fluids to the patient; Deviation/falling of the ventricular septal defect blocker from position: Close monitoring is required during and after technical manipulation to take appropriate intervention measures; Causes conduction block: The doctor needs to closely monitor, promptly detect bradycardia and atrioventricular block for treatment; Other complications: The puncture site is bleeding or infected: It is necessary to monitor and manage according to the general intervention procedure.
3. Atrial septal defect sealing technique

3.5 Common complications and treatment Pericardial effusion : Due to tearing, perforation of the atrial wall or atrial appendage,... due to technical manipulations. The treatment is early detection, early drainage and early contact with the surgeon; Embolism due to thrombus or air: The doctor should pay attention to anticoagulation and expelling gas; Hemolysis: Due to residual shunt. This is a rare condition that requires close monitoring and adequate perfusion; Complications of displacement or fall of the atrial septal defect from its position: It is necessary to closely monitor the patient in order to promptly appoint a re-surgery; Other complications: Bleeding, infection, ... at the puncture site. Treatment measures are monitoring and intervention in accordance with the standard regimen. The procedure for occluding the ventricular septal defect and Atrial septal defect is a relatively complicated technique. When assigned to perform this technique, patients need to strictly follow all instructions of the doctor to reduce the risk of complications and ensure effective treatment.
To protect cardiovascular health in general and detect early signs of myocardial infarction and stroke, customers can sign up for Cardiovascular Screening Package - Basic Cardiovascular Examination of Vinmec International General Hospital . The examination package helps to detect cardiovascular problems at the earliest through tests and modern imaging methods. The package is for all ages, genders and is especially essential for people with risk factors for cardiovascular disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














