This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
The association between the increased prevalence of gastroesophageal reflux disease (GERD) and obesity has generated great concern about the association between the two conditions. Several studies have addressed a potential relationship between GERD and obesity, but the exact mechanism by which obesity causes reflux disease has not been clearly defined.
1. Frequency of reflux esophagitis in obese patients
Gastroesophageal reflux disease (GERD), with its symptoms proven to reduce quality of life (QoL), appears to represent an important variation in morbidity. When defined as at least weekly heartburn and/or acid reflux, prevalence in the Western world typically ranges from 10% to 20% while in Asia the prevalence is reported is less than 5%. Longitudinal studies have addressed several risk factors for GERD, and indeed obesity is considered a potential risk factor.
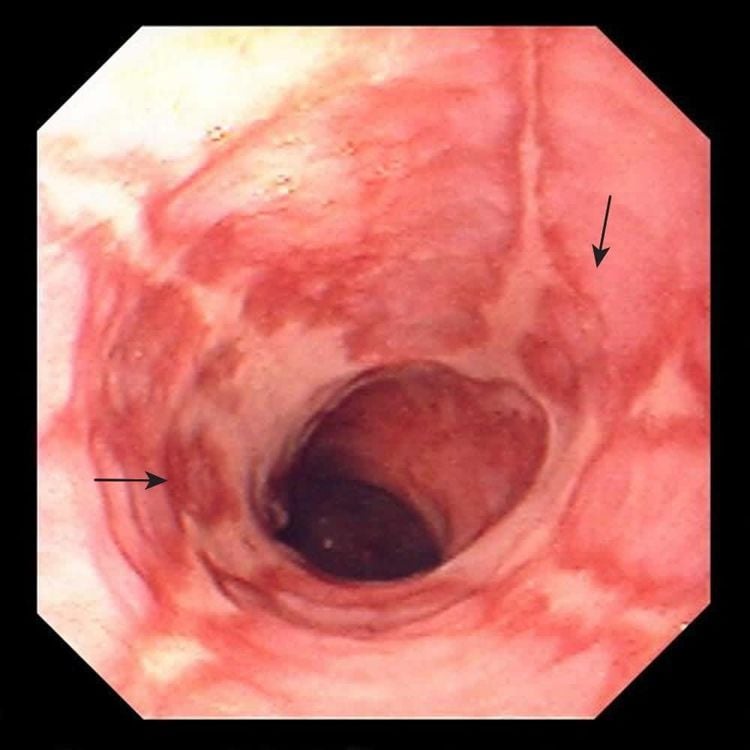
Interestingly, obesity, commonly defined as a body mass index (BMI) > 30, has increased to epidemic levels in some parts of North America, Europe and Asia. A confluence of increases The increased prevalence of GERD, symptomatically, erosive esophagitis, Barrett's esophagus (BE), esophageal adenocarcinoma, and obesity have generated great concern about the association between these two conditions and underlying mechanisms underlying this association.
2. Potential Relationship Between GERD and Obesity
Several studies have focused on the potential relationship between GERD and obesity, and the results obtained from those investigations have shown that obesity is associated with an increased risk of both symptoms and GERD complications, i.e. erosive esophagitis, Barrett's esophagus, and esophageal adenocarcinoma compared with those with normal BMI. There is also some degree of dose-dependent relationship between BMI and GERD-related disorders and, moreover, a recent large cohort focusing on adult women reported an increased risk of GERD. with a higher BMI is possible. normal range.
3. Why does obesity cause reflux esophagitis?
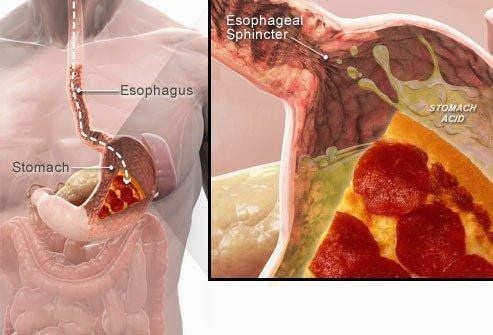
Even though some mechanism by which obesity causes reflux disease has been proposed, the commonly suggested pathogenesis is that increased intra-abdominal pressure relaxes the lower esophageal sphincter (lower esophageal sphincter). ), thereby exposing the lining of the esophagus to gastric juice. The results of 24-hour pH monitoring studies suggest that obesity is associated with a significant increase in the number of reflux episodes, as well as prolonged reflux episodes and duration of pH <4, particularly. especially in the postprandial period. This finding was confirmed, in a more recent study, also by monitoring of pH impedance: not only did acid reflux but the number of times without acid reflux increased significantly as BMI increased.
A recent study to evaluate pressure morphology and function of the esophagogastric junction, using high-resolution manometry, reported that due to obesity, pressure gradients Gastro-oesophageal force is altered in a way that promotes reverse flow of gastric contents into the esophagus.
4. Waist circumference and gastro-oesophageal pressure difference
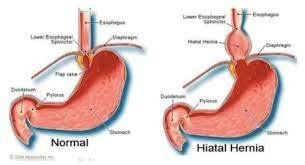
Both intragastric pressure and gastroesophageal pressure gradient were clearly correlated with both BMI and waist circumference, but when they were analyzed simultaneously in a regression model, waist circumference were found to be independently associated with different pressure gradients, while the relationship between BMI and pressure became insignificant or decreased significantly. In addition to the abnormal pressure gradient, high-resolution measurements also suggest that obesity is associated with diaphragmatic hernia.
There is a significant correlation between BMI, waist circumference and axial separation of the intrinsic lower esophageal sphincter and the internal diaphragm, and this is thought to be indicative of pressure stress. due to increased pressure in the stomach. In agreement with this finding, in a retrospective case-control study evaluating BMI in relation to esophagitis and diaphragmatic hernia, it was found that obesity was strongly associated with the combined occurrence of esophagitis. esophagus and diaphragmatic hernia.
It is widely acknowledged that hiatal hernia has several pathophysiological effects in the pathogenesis of GERD: increased frequency of stress-induced reflux, decreased lower esophageal sphincter pressure, decreased clearance esophageal acidosis and increased susceptibility to transient lower esophageal sphincter relaxation.
5. The role of the lower esophageal sphincter
Among the mechanisms that cause reflux, the mechanism of relaxation of the lower esophageal sphincter plays the most important role. The standard, postprandial reflux pattern has recently been evaluated in obese and overweight patients using a combination of 2-hour postprandial esophageal manometry and esophageal pH monitoring. The results of this study showed that, during the postprandial period, both obese and overweight patients had a significant increase in the rate of lower esophageal sphincter relaxation and lower esophageal sphincter relaxation rate. have acid reflux compared to those with normal BMI.
Both BMI and waist circumference showed a significant positive correlation with lower esophageal sphincter relaxation and a dose-effect relationship. It is therefore likely that higher postprandial intragastric pressure induces stronger stimulation of both tension and stretch receptors in the proximal stomach, leading to greater postprandial relaxation of the lower esophageal sphincter.
6. Proposed mechanisms by which abdominal obesity causes reflux
| Yếu tố cơ học | Tăng chênh lệch áp lực trong dạ dày và dạ dày-thực quản |
| Tăng nguy cơ thoát vị khe hoành | |
| Tăng độ nhạy đối với giãn cơ thắt thực quản dưới | |
| Giảm áp lực cơ thắt thực quản dưới | |
| Yếu tố sinh học phân tử | Tăng mức độ adipocytokine bao gồm interleukin 6 và yếu tố hoại tử khối u α |
| Rối loạn vận động | Tốc độ làm trống dạ dày bị chậm lại và thời gian làm sạch thực quản bị chậm lại |
7. Abdominal obesity
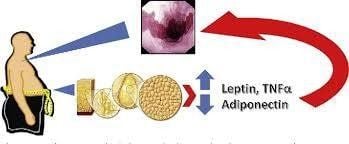
Belly fat or visceral fat, ie abdominal obesity (VAT) is very different from peripheral fat or subcutaneous fat (SCAT). For example, abdominal obesity is more metabolically active, characterized by higher numbers of immune and inflammatory cells, and more insulin resistant, thus leading to a higher overall mortality rate for obesity. subcutaneous fat
Abdominal obesity may better explain some of the epidemiological features of Barrett's esophagus and adenocarcinoma of the esophagus. Body fat distribution tended to be more visceral than amputation in groups at high risk of Barrett's esophagus.
A recent study showed that abdominal diameter as measured by waist circumference was a risk factor for Barrett's esophagus independent of BMI, while the association between BMI and Barrett's esophagus disappeared after Adjust belly diameter. These studies indicate that abdominal fat is the main factor linking obesity and Barrett's esophagus. In addition to mechanical stress, visceral fat is metabolically active and is clearly associated with serum levels of adipo-cytokines including interleukin 6 and tumor necrosis factor α, which may play a role in GERD and/or consequent carcinogenesis.
In fact, in a very recent study, a large amount of visceral belly fat relative to subcutaneous fat was found to be associated with a significant increase in the risk of Barrett's esophagus.
8. Results of the studies
Considering the dose-response relationship between obesity and the occurrence of GERD and/or the resulting complications, an inverse relationship between weight loss and GERD symptoms would be expected. The prevalence of GERD symptoms in overweight and obese subjects as well as the impact of weight loss on GERD symptoms were evaluated in a recent prospective study. Weight loss strategies include dietary changes, increased physical activity as well as behavioral changes. The results obtained from the study showed that weight loss led to a significant improvement in GERD symptoms, thus considering weight loss as an important lifestyle change in the treatment of GERD. Furthermore, weight loss over a 6-month period, was associated with a reduction in GERD symptoms in 81% of patients and complete resolution in 65% of patients. This finding provides support for recommending weight loss as the primary treatment for overweight reflux patients, however, unfortunately this clinically important finding has not been described to date.
More research is needed on the long-term effects of weight loss on the occurrence of reflux and the reduction of reflux symptoms before any firm conclusions can be drawn about the ultimate beneficial effects of weight loss.
9. Conclusion
Obesity appears to be associated not only with the development of GERD symptoms but also with GERD complications such as erosive esophagitis, Barrett's esophagus, and adenocarcinoma of the esophagus.
Although there is substantial evidence confirming an important role of increased esophageal-gastroesophageal pressure gradient and inflammatory mediator production by abdominal adipose tissue in the pathogenesis of GERD, there is an interplay between obesity and GERD remain unclear. Furthermore, weight loss appears to reduce GERD symptoms but further studies are being done to better understand the exact mechanism by which obesity causes reflux disease in order to identify and establish treatments. new treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. [PMC free article] [PubMed] [Google Scholar] Corley DA, Kubo A. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. AmJ Gastroenterol. 2006;101:2619–2628. [PubMed] [Google Scholar] Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. [PubMed] [Google Scholar] Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211. [PubMed] [Google Scholar] Sara Emerenziani, Maria Paola Rescio, Michele Pier Luca Guarino, and Michele Cicala, Gastro-esophageal reflux disease and obesity, where is the link? World J Gastroenterol. 2013 Oct 21; 19(39): 6536–6539.