This is an automatically translated article.
Posted by Doctor La Thi Thuy - Cardiovascular Center - Vinmec Central Park International General HospitalAortic valve stenosis accounts for 2% of cardiovascular disease and is the most common cause of left ventricular ejection fraction obstruction. The most common acquired causes of aortic stenosis are rheumatic heart disease and fibro-calcium degeneration of the aortic valve in the elderly. This is the most common valvular disease, accounting for one-quarter of all heart valve disease cases with 80% of patients with aortic stenosis being male (male:female ratio is 2:1)
1. Symptoms of aortic stenosis 1.1. Functional symptoms These symptoms usually only appear when the aortic valve stenosis is severe
Chest pain: When the myocardial oxygen demand increases, the heart muscle weakens due to increased blood pumping through the valve. narrow heart after a long time. Chest pain due to coronary artery disease. Dizziness, syncope: This symptom occurs due to a fixed obstruction of the ejection path from the left ventricle, reducing the ability to increase cardiac output. The patient may experience a severe drop in blood pressure leading to dizziness or fainting. Heart failure: Due to dysfunction of systolic or diastolic function. Cardiac fibrosis leads to decreased contractility of the heart. Compensatory mechanisms to increase intravascular volume will increase left ventricular pressure, increase pulmonary capillary pressure causing pulmonary stasis. 1.2. Physical symptoms Pulse palpation: The prominent symptom is a weak to slow bouncing carotid pulse
Palpable systolic fibrillation in the right II intercostal space. In addition, the apex of the heart can be palpated with a wide, diffuse beat if the left ventricle is enlarged.
Auscultation: The main pathological sounds include
systolic ejection in the upper right side of the sternum, spreading to the neck and reaching the highest intensity in the head - mid-systole. The more severe the aortic stenosis, the longer, louder, and slower the murmur. T1 and T2 sounds do not change with aortic stenosis The T3 sound is indicative of poor left ventricular systolic function. The T4 sound occurs because the left atrium contracts to force blood into the left ventricular chamber, which is poorly dilated when the aortic valve is tight. In addition, murmurs of aortic regurgitation may be heard due to stenosis often associated with regurgitation. Resting tachycardia in patients with severe aortic stenosis is one of the first signs of low cardiac output.
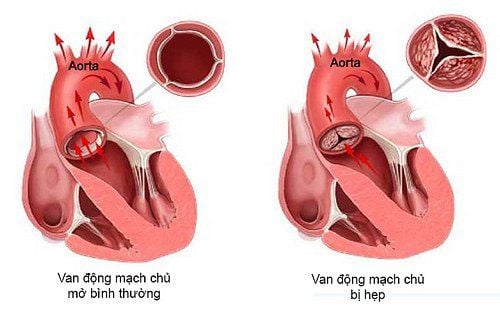
Hình ảnh mô tả tình trạng hẹp van động mạch chủ
2. Definite diagnosis of aortic stenosis The definitive diagnosis of aortic stenosis is mainly based on clinical and echocardiographic findings.
2.1 Clinically: Includes physical symptoms and signs.
2.2 On clinical examination: Electrocardiogram:
Usually left atrial hypertrophy (80%) and left ventricular hypertrophy (85%). Arrhythmias rarely occur, mainly in the late stages and most often in atrial fibrillation, especially in the presence of mitral valve disease. Atrioventricular block can occur when an aneurysm abscess is complicated by endocarditis
Chest X-ray:
Little diagnostic value because the image may be completely normal. Heart shadow resembles a boot if left ventricular hypertrophy is concentric. The heart shape is usually enlarged if left ventricular dysfunction is present or there is an associated HoC. Some other images that can be encountered are calcification of the aortic valve in the elderly (tilt film) or dilated posterior ascending aortic stenosis.
Doppler echocardiography:
helps diagnose and evaluate the degree of aortic stenosis through the calculation of the area of the aortic orifice and the measurement of the transaortic valve differential pressure by Doppler:
Mild valve stenosis aorta (valvular orifice area > 1.5 cm2, maximal transvalvular gradient < 40 mmHg, mean gradient < 20 mmHg) Moderate stenosis (orifice area 1 to 1.5 cm2, maximal gradient maximum 40-70 mmHg, mean gradient 20-40 mmHg) Tight stenosis (valvular orifice area < 1.0 cm2, maximal gradient > 70 mmHg and mean gradient > 40 mmHg)

Siêu âm Doppler tim giúp các bác sĩ chẩn đoán và đánh giá tình trạng hẹp van tim
Transesophageal echocardiography: Can directly measure the orifice area (2D), but it is more difficult to obtain a Doppler spectrum of flow through the narrowed valve. This tool is very useful to evaluate aortic valve morphology in congenital aortic stenosis
Stress ultrasound: to distinguish true aortic stenosis with systolic dysfunction severe left ventricular (so the transvalvular pressure gradient is low) with cases of pseudo-stenosis (disease affecting the myocardium, with mild aortic stenosis, so also left ventricular systolic dysfunction and gradient low transaortic valve) because the case of pseudo-stenosis did not improve after surgery. Dobutamine is infused in increments of 5 to 20 mg/kg/min to gradually increase cardiac output, followed by echocardiography to measure valvular orifice area and transaortic pressure gradient gradually. The test should be stopped immediately when the patient has hypotension, chest pain, or arrhythmias
3. Treatment of aortic stenosis The treatment of aortic stenosis depends on the severity (severe) ) of aortic valve injury. Specifically:
If it is mild or moderate aortic stenosis, the patient needs to be monitored for a while by cardiologists, the patient will be checked periodically (including blood tests and echocardiography) every 6 months - 1 year, depending on the doctor's assessment of the condition or as soon as any symptoms appear. Medical treatment of aortic stenosis is only a temporary treatment, including treatment of symptoms and treatment of complications, if any (treatment of angina pectoris, treatment of heart failure, treatment of embolism, disorders of the heart). arrhythmia, bacterial endocarditis...)
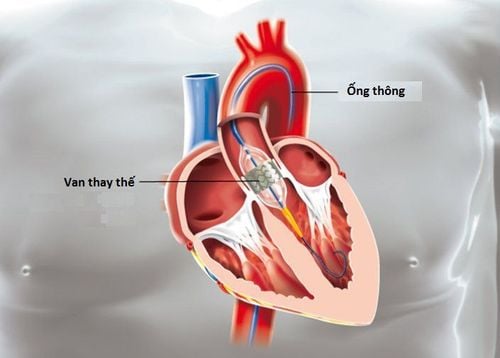
If severe aortic stenosis is accompanied by symptoms (clinical and/or exercise findings), the patient is indicated for aortic valve replacement. Aortic valve replacement surgery (SAVR) was once considered the gold standard in the long-term treatment of aortic stenosis, but with an increasing number of elderly and aging patients, the surgery has been heavily modified. To minimize invasiveness such as choosing a minimally invasive surgical approach and choosing next-generation prosthetic valves to improve prognosis, percutaneous aortic valve replacement (TAVI) was introduced for the first time. started in 2002 further reduces surgical trauma and avoids cardiac arrest complications as well as cardiopulmonary bypass. Since it was approved by the US Food and Drug Administration (FDA) in 2011, more than 100,000 patients have received TAVI worldwide. Recently, with technological developments in the valve and guide systems, the TAVI procedure has grown worldwide. Currently, the trend in the world is to replace valves in both moderate or low risk patients. The latest publications show comparable efficacy between the two treatments based on the primary endpoint of death and nonfatal stroke. The effect of reducing cardiovascular symptoms at 2-year follow-up was the same.

Hình ảnh can thiệp tim mạch tại Bệnh viện Đa khoa Quốc tế Vinmec
Patients with aortic stenosis can choose to be treated at Vinmec International General Hospital. At Vinmec Central Park Hospital, 70 cases of aortic valve replacement (TAVI) have been performed for patients with aortic stenosis over the past 2 years with high success. The hospital is also the only one in the country that has obtained an independent TAVI performance certificate so far. Here gathers a team of Cardiologists including professors, doctors, masters, specialists 2 experienced, with great reputation in the field of medical treatment, surgery, cardiac catheterization. intervention. Vinmec also focuses on applying advanced techniques in the diagnosis and treatment of cardiovascular diseases, using a system of modern medical equipment that meets international standards.
For detailed advice on treatment methods for aortic valve stenosis, you can go directly to Vinmec medical system or register online HERE