This is an automatically translated article.
Posted by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital
Myasthenia gravis is an autoimmune neuromuscular disease that causes fluctuating muscle weakness in the eyes, medulla oblongata, and limbs and can, in 15% of cases, cause myasthenia gravis, a characteristic neurological emergency. by respiratory failure. Although uncommon, myasthenia gravis needs to be diagnosed and treated quickly because of the high likelihood of improvement and remission. In particular, the diagnosis and treatment of myasthenia gravis in pregnant women and children has special notes.
1. Muscle weakness in pregnant women
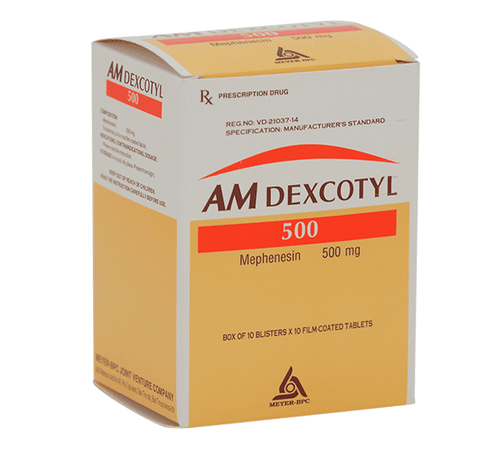
Special precautions are taken when treating women of childbearing age and during pregnancy. While pregnancy outcomes for mothers with myasthenia gravis are generally excellent, 20% to 30% of women may experience an exacerbation, mostly during the first trimester or in the postpartum period. Improvement is possible in the second and third trimesters. Ideally, women planning to become pregnant should discuss a treatment plan and review risks with their neurologist prior to becoming pregnant and wait for medication adjustments if needed. The goals should be to minimize myasthenic symptoms and the risk of maternal exacerbations and to avoid the potential for adverse fetal exposure to immunosuppressants. Pyridostigmine, IVIg, plasmapheresis, and prednisone are generally safe during pregnancy, whereas mycophenolate mofetil has a clear risk of fetal malformation and should be avoided during pregnancy (Table 1).
Nhược cơ ở phụ nữ mang thai có thể gây dị tật bẩm sinh
There may be fatigue in the second stage of labor, and labor may be prolonged and there may be fetal distress. The obstetrician should be prepared to use forceps or vacuum aspiration during this period if needed. Neostigmine 1.5 mg IM or 0.5 mg IV is equivalent to 60 mg of oral pyridostigmine and can be used if needed during delivery. Myasthenia gravis by itself is not an indication for cesarean section - like any other surgery, it can cause an exacerbation of myasthenia gravis and should be reserved for obstetric indications.
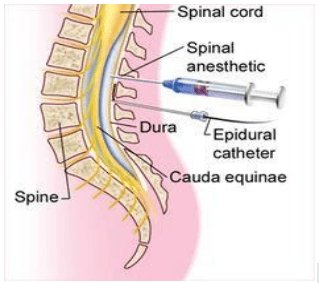
Patients with myasthenia gravis are more sensitive to anesthetics, anaesthetics, and non-depolarizing muscle relaxants and should be particularly avoided as they can cause severe and prolonged muscle weakness. For women with myasthenia gravis, an epidural is the anesthetic method of choice for delivery.
Gây tê ngoài màng cứng là phương pháp vô cảm được lựa chọn cho cuộc đẻ ở phụ nữ mang thai ngoài màng cứng
Magnesium for the treatment of eclampsia should be used with caution in women with myasthenia gravis because of its negative effect on neuromuscular transmission and potential for muscle weakness. Maternal mortality has been reported from magnesium use in pregnant women with myasthenia gravis.
Table 1 . Treatments in pregnant and lactating women
2. Children's weakness
Myasthenia gravis in children is rare, and is more difficult to diagnose, in part because of the higher prevalence of seronegative and likely differential diagnosis of genetic myasthenic syndromes. Juvenile, or childhood, myasthenia gravis is an acquired autoimmune postsynaptic disease of neuromuscular transmission that occurs in prepubertal patients and shares most of the clinical features and response to treatment, such as weakness. acquired in adults. It should be differentiated from genetic forms of neuromuscular conduction defects (congenital myasthenic syndromes). Treatments for myasthenia gravis are similar to those in adults and are often very effective with a high remission rate. Evidence-based guidelines are lacking in this group because treatment trials for myasthenia gravis have excluded patients younger than 18 years of age and because of the rarity of the disease in this age group. The role and timing of thymectomy, while well defined in adult myasthenia gravis, remains unknown or standardized in children. Thymectomy is often considered as a treatment option for children with seronegative systemic myasthenia gravis when the response is inadequate to pyridostigmine and other immunosuppressive agents or to avoid adverse effects. prolongation of immunosuppressants, especially prednisone, in very young patients. In children with seronegative systemic myasthenia gravis, the role of thymectomy is even less clear and necessitates the exclusion of a congenital myasthenic syndrome. While acquired ocular myasthenia gravis has a high rate of spontaneous remission, myasthenia gravis can be refractory to treatment in Asian and African-American children and often results in fixed ocular muscle weakness requiring correction. surgical correction. myasthenia gravis in children should be initiated with pyridostigmine; Immunosuppressive agents should be considered in difficult-to-treat cases, and prednisone should be used at the lowest possible dose because of growth retardation, bone mineral depletion, and disruption of immunization schedules in young children. IVIg is generally the preferred treatment option in this age group.

Nhược cơ ở trẻ em rất khó chẩn đoán
Transient neonatal myasthenia gravis is a transient form of autoimmune myasthenia gravis seen in infants of mothers with autoimmune myasthenia gravis, and it is caused by placental transmission of maternal AChR antibodies. It resolves on its own after maternal antibodies are cleared, usually within 1 month, and with supportive therapy only. It is very rare, occurring in 10% to 15% of babies born to mothers with myasthenia gravis. Although very rare, it should be considered in the differential diagnosis of floppy infant syndrome, and all children of mothers with myasthenia gravis should be monitored for signs of muscle weakness and especially functional impairment. respiratory and medullary functions (weak crying, poor feeding). Onset of symptoms is usually between 12 and 48 hours postpartum, with that delay due to mother-to-child transmission of α-fetoprotein, its immunosuppressive effects, or anticholinesterase agents.
The effect of maternal antibodies on the fetus can also rarely cause congenital polyarticular spasticity, which can lead to intrauterine or neonatal death and may even be seen in the fetus of the mother. mothers with no symptoms. Congenital polyarticular stiffness in myasthenia gravis has a high risk of recurrence and requires pre-pregnancy counseling. Maternal myasthenia gravis should always be considered in the differential diagnosis of congenital polyarticular stiffness.

Cứng đa khớp bẩm sinh có nguy cơ cao tái diễn và cần được tư vấn trước khi mang thai
To register for examination and treatment at Vinmec International General Hospital, you can contact the nationwide Vinmec Health System Hotline, or register online HERE.
Source: Emma Cifaloni. Myasthenia Gravis and Congenital Myasthenic Syndromes. Continuum (Minneap Minn) 2019; 25 (6, Muscle and Neuromuscular Junction Disorders): 1767-1784.