This is an automatically translated article.
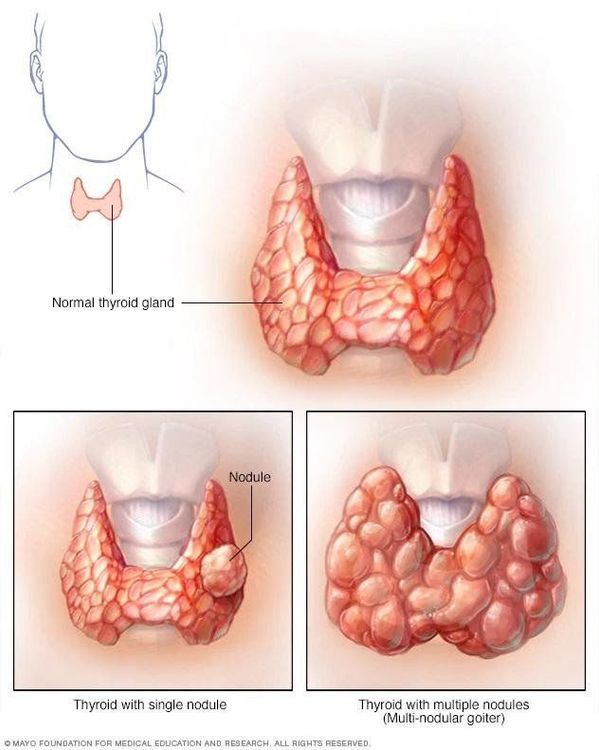
The article was written by Dr. MSc Nguyen Thuc Vy - Doctor of Radiology, Department of Diagnostic Imaging - Vinmec Nha Trang International General HospitalMultinodular goiter (also called multinodular goiter) is defined as a large thyroid gland with many thyroid nodules with thyroid function that can be normal, decreased or increased.
1. Introduction
A thyroid nodule (also known as a thyroid nodule or a thyroid nodule) is a lesion in the thyroid gland that is distinct in imaging from the surrounding normal thyroid parenchyma.In terms of the term "multi-nodular thyroid" is a term that has been criticized for being somewhat unreasonable because in some cases the thyroid gland has many nodules but is not large, leading to its widespread use than the term "Human Armor" or "Multiple Armor".
Polygranulomatous aneurysm is common in women (M: F = 1: 3) between the ages of 35-50. Patients usually have normal (parathyroid) thyroid function but may also have decreased or increased thyroid function, resulting in systemic symptoms of hypothyroidism or hyperthyroidism, respectively.
When there is an overactive thyroid (hyperthyroidism) the condition is called toxic multinodular goiter (toxic multinodular goiter) or Plummer's disease.
2. Pathology
Pathologically, multinodular aneurysms develop from a simple aneurysm (large thyroid gland without any nodules) as a result of repeated stimulation and response.Simple goiter is seen in many pubertal boys and girls, and is almost a physiological response to the complex hormonal changes occurring at this time. It usually regresses, but sometimes (more commonly in girls) it persists and develops further during pregnancy.
Most simple thyroid aneurysms develop into multinodular thyroid nodules over time. Thyroid nodules develop gradually over a period of several years, then become stable and less prone to further growth. Rarely, a noticeable spontaneous decrease in the size of the thyroid gland has occurred. Sometimes, there is a sudden increase in the size of the gland accompanied by sharp pain in one area. This event suggests hemorrhage in the thyroid nodule and can be confirmed by ultrasonography. Within 3-4 days, symptoms subside, and within 2-3 weeks, the thyroid gland may return to its previous size. In such a situation, acute thyrotoxicosis may develop and subside spontaneously.
Most (>90%) of these nodules are benign, hyperplastic nodules or adenomas with varying degrees of cystic degeneration. The presence of serum or colloidal fluid in the thyroid nodules may be noted.
Only a small fraction (4-6.5%) of thyroid nodules are at risk of malignancy. Family history of malignancy and previous exposure to cervical radiation are risk factors for malignant thyroid nodules.

3. Ultrasound imaging characteristics
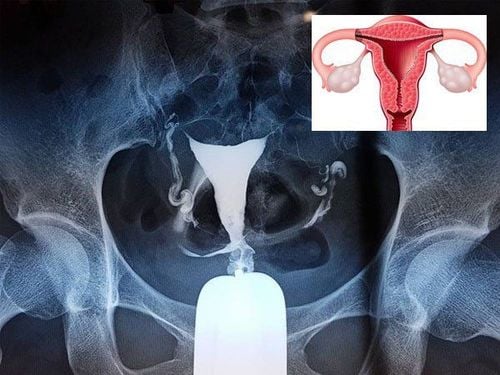
Ultrasonography is the primary imaging modality to screen for nodules and to look for suspicious signs of malignant changes in thyroid nodules.Normally, benign thyroid nodules have the following features: Homoelyhyperechoic; Ambient hypoechoic halo border Spongy or honeycomb; cystic component containing colloidal fluid with cometoidal echogenic foci Lime Ovarian cystic or coarse Doppler calcification: peripheral vessels are often noted, may show central nodular hyperperfusion (mainly in hyperfunctioning nodules) Important to screen for presence of malignant features (if present) in any nodule and fine-needle aspiration cytology (thyroid FNA) can be performed with suspected nodules.
Signs suggestive of malignancy on ultrasound: Very hypoechoic solid nodule Presence of intranodular microcalcifications Spread of lesion beyond thyroid border Metastasis to cervical lymph nodes Nodules have a larger shape and height width in cross section (vertical axis thyroid nodule) Less specific sonographic findings that may suggest malignancy include absence of halo border, indistinct or irregular margins, solid component, and increased vascularity center. The probability of malignancy increases with the number of suspicious features on ultrasound.
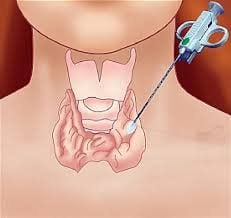
4. When to perform fine needle aspiration (FNA)
FNA is considered the gold standard test to evaluate thyroid nodules. This is an in-clinic procedure, done with a 23G to 27G fine needle, to take a tissue sample for cytology examination. It is a safe, accurate and cost-effective way to assess thyroid nodules.FNA can be performed by palpation or with ultrasound guidance. An ultrasound machine with a frequency probe from 7.5 to 10 MHz provides a clear and continuous image of the thyroid gland and allows real-time visualization of the needle tip to ensure accurate sampling. Ultrasound-guided FNA is preferred for palpable nodules.
Indication of FNA based on thyroid nodule size and ultrasound characteristics (according to the guidelines of the American Thyroid Association ACR TIRADS 2017):
Multiply ≥ 1cm with high suspected ultrasound features Multiply ≥ 1.5 cm with moderate sonographic features Nodules 2.5 cm with low suspicion For nodules that do not meet the above criteria FNA is not needed (with some exceptions) and nodules pure cystic form.
5. Treatment
5.1 Treatment of benign nodules If the thyroid nodule is not cancerous, treatment options include:Watchful waiting : If a biopsy shows you have a noncancerous thyroid nodule, your doctor may recommend Recommend just monitor your status. This usually means regular physicals, ultrasounds, and thyroid function tests. You may also have to have another biopsy if the nodule grows larger. If the benign thyroid nodule does not change, you may never need treatment. Thyroid hormone therapy: If your thyroid function tests show that your thyroid is not producing enough thyroid hormone, your doctor may recommend thyroid hormone therapy. Surgery: A noncancerous nodule can sometimes require surgery if it's so large it's hard to breathe or swallow. Nodules diagnosed as unspecified or suspected by biopsy also require surgical removal so that signs of cancer can be checked. Radiofrequency ablation of thyroid nodules (RFA): A non-surgical thermal tumor destruction method being applied at Vinmec. 5.2 Treating nodules that cause hyperthyroidism If the nodule is producing thyroid hormone, overloading the thyroid's normal hormone production, your doctor may recommend treatment for hyperthyroidism. This may include:
Radioactive Iodine : Doctors use radioactive iodine to treat hyperthyroidism. Taken as a capsule or in liquid form, radioactive iodine is absorbed by your thyroid gland. This causes the nodules to shrink and the signs and symptoms of hyperthyroidism to subside, usually within 2 to 3 months. Antithyroid drugs: In some cases, your doctor may recommend an antithyroid medication such as methimazole (Tapazole) to relieve the symptoms of hyperthyroidism. Treatment is generally long-term and can have serious side effects on your liver, so it's important to discuss the risks and benefits of treatment with your doctor. Surgery: If treatment with radioactive iodine or antithyroid drugs is not an option, your doctor may recommend surgery to remove an overactive thyroid nodule.

Alcohol injection into the thyroid nodule : Another option to control some small cancerous nodules. This technique involves injecting a small amount of alcohol into the cancerous thyroid nodule to destroy it. Often requires multiple treatments.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles source references: radiopaedia.org, NCBI, mayoclinic.org